Our Addiction Resources
Navigating the world of addiction and recovery can be overwhelming. We’re here to provide clear, compassionate education and guidance. From practical advice for maintaining sobriety to informational guidance on the long-term effects of substance abuse, our content is a beacon of hope and understanding.
Our Team is Ready are ready to take your call
Call us Today!
or we can call you. Fill out form below
Our Blog

What Is Pink Cocaine?
Called pink cocaine based on its appearance, this dangerous designer drug in fact rarely contains cocaine. The party drug is made from a mix of substances like ketamine, MDMA, and other illegal drugs.
While it’s grown in popularity, especially in the U.S., it poses serious health risks due to its unpredictable contents and effects. Often sold under various names like tusi, tuci, and tucibi, it’s not actually cocaine, despite what the name suggests.
What Is Pink Cocaine Made Of?
Pink cocaine is a synthetic drug often mixed with various substances, like a drug cocktail. Often, pink cocaine includes a combination of MDMA, methamphetamine, and ketamine, a dissociative. It can include cocaine as well. Pink cocaine is typically dyed pink with food coloring, giving it its distinct pink powder appearance.1
In some cases, it may even contain opioids or new psychoactive substances (NPS), making its effects even more unpredictable. NPS are synthetic drugs designed to mimic the effects of known drugs but are chemically different, often leading to dangerous and unexpected outcomes. Additionally, batches of pink cocaine are sometimes laced with other harmful substances like benzodiazepines or bath salts.1
Since pink cocaine is made in illegal and unregulated labs, its exact contents vary, making it difficult for users to know what they are consuming.
How Is Pink Cocaine Used?
Pink cocaine is a recreational drug commonly found in the club scene that is usually consumed by snorting or sometimes ingesting it orally. The stimulant effects people experience depend on the specific mix of substances and how much they take.
Since pink cocaine often contains a mix of stimulants like MDMA and depressants like ketamine, it can cause a range of sensations, from excitement to deep relaxation. This mix of drugs is sometimes referred to as a “speedball” because it combines opposing effects.
Users often report feeling a rush of euphoria, increased energy, heightened sensory perception, and dissociation from their body within an hour or two of taking it. However, since the drug’s effects depend on its composition, how much is taken, and the person’s tolerance, the user’s reactions can be unpredictable. Some people might feel a boost in their heart rate and happiness, while others could experience a slower, more sedated high.1
The effects typically peak within 1-3 hours, but users may still feel the effects lingering for up to 8 hours, depending on the substances in the mix. Because different batches of pink cocaine vary so widely, it’s impossible to predict exactly how someone will react, making it a risky substance to use.1
Effects of Pink Cocaine
Pink cocaine can cause anything from mild confusion to life-threatening symptoms. In small amounts, some users report mild euphoria, increased alertness, and enhanced sensory perception. However, the negative effects can be severe, and users may experience the following:1
- Agitation or aggressive behavior
- Confusion or disorientation
- Visual or auditory hallucinations
- Nausea or vomiting
- Anxiety or paranoia
Physical side effects might include:1
- Increased heart rate and blood pressure
- Breathing difficulties
- Low body temperature
- Seizures
A particularly dangerous effect of pink cocaine is the potential for excited delirium, a state where the user becomes highly agitated, which can lead to cardiac arrest and sudden death if not treated immediately.
Long-term use of pink cocaine can cause more lasting damage. The combination of drugs like ketamine and MDMA in pink cocaine can harm the heart and blood vessels. It can also alter brain chemistry, leading to memory problems, sleep disturbances, anxiety, and depression over time. Chronic use may also affect focus and make it harder to function in daily life.
Addiction Potential of Pink Cocaine
Like many other illegal substances, pink cocaine has a high potential for addiction. Since it often includes highly addictive drugs like MDMA, methamphetamine, and even opioids, users can quickly develop a tolerance to it. This means that over time, they will need to take larger doses to achieve the same high. The more frequently a person uses pink cocaine, the higher the risk of dependence and addiction.
As tolerance builds, users may also experience withdrawal symptoms if they stop using the drug, making it harder to quit. These withdrawal symptoms might include anxiety, depression, and intense cravings, which can compel users to continue using despite knowing the risks.
One of the biggest concerns with pink cocaine is the unpredictability of its contents. Users never know the exact strength of the dose or what substances they’re ingesting. This unpredictability increases the risk of accidental overdose, especially if the batch contains dangerous opioids like fentanyl, which have been found in some samples of pink cocaine.

Getting Help for Pink Cocaine Addiction
If you or someone you love is struggling with an addiction to pink cocaine, it’s important to know that help is available. Due to the complex and dangerous nature of pink cocaine, professional help is crucial.
1. Assess Personal Readiness
Start by acknowledging the impact of pink cocaine on your life. Taking time to reflect on how the drug has affected your health, relationships, and well-being can be a powerful motivator to seek help. It’s okay if you feel uncertain—just recognizing the need for change is a big step.
2. Contact a Healthcare Professional
Reach out to a doctor or addiction specialist who can evaluate your situation and discuss treatment options. They may suggest starting with a medically supervised detox, especially because pink cocaine often includes substances like ketamine and opioids. Detoxing under medical care helps manage withdrawal symptoms safely and effectively.
3. Explore Treatment Programs
Research available inpatient or outpatient treatment programs to find one that fits your needs. Inpatient rehab offers a structured environment with round-the-clock support, which is ideal for individuals who need intensive care. Outpatient programs provide flexibility, allowing patients to receive therapy while continuing their daily routines. Each program type offers therapy, counseling, and support to build healthier coping mechanisms.
4. Begin Behavioral Therapy
Behavioral therapy, such as cognitive behavioral therapy (CBT), is essential in addiction treatment. Working with a therapist can help identify thought patterns and habits that fuel addiction. You’ll learn practical strategies to manage cravings, navigate triggers, and build confidence to handle life without relying on drugs.
5. Address Co-Occurring Conditions
Pink cocaine addiction can often come with other mental health challenges, like anxiety or depression. Dual diagnosis treatment addresses both substance use and mental health issues simultaneously, increasing the chances of lasting recovery. Speak with your treatment provider about finding a program that can treat co-occurring disorders effectively.
Start Your Journey to Recovery with Lumina Recovery
Pink cocaine is a dangerous, unregulated designer drug that poses significant health risks. Its unpredictable composition, combined with the addictive nature of the substances it contains, makes it a risky choice for anyone. The best way to avoid these risks is not to use pink cocaine at all, but for those who struggle with addiction, there is help available through treatment programs and support systems.
At Lumina Recovery, we provide medically supervised detox and comprehensive addiction rehabilitation programs, tailored to each individual’s needs. Our personalized approach includes dual diagnosis care and a variety of therapeutic treatments.
If you or someone you know is struggling with pink cocaine addiction, contact us today to learn about your treatment options.
Source:

Relapse Triggers to Watch for This Holiday Season
The holiday season is a time of joy, connection, and celebration, but for individuals in recovery, addiction and the holidays can create a difficult combination. Family gatherings, changes in routine, and an abundance of social events where alcohol and other substances are present can make staying sober more challenging.
Understanding the common relapse triggers and having strategies to manage them can help you or your loved one maintain sobriety during the holidays.
Here are some of the most common holiday relapse triggers and suggestions on how to cope with them.
1. Social Pressure to Drink or Use Substances
Social gatherings during the holiday season often revolve around alcohol or other substances, making them a common alcohol relapse trigger for those in recovery.
Whether it’s a festive family dinner, a workplace celebration, or a New Year’s Eve party, there’s a high likelihood that people will be drinking or using substances. This can create a challenging environment where it’s easy to feel left out or pressured to join in.
The key to handling social pressure is preparation. Plan ahead by bringing your own non-alcoholic drinks or mocktails, so you can blend in without feeling uncomfortable. If you’re worried about questions or comments, have a simple explanation prepared, like “I’m not drinking tonight” or “I’m focusing on my health.” If you’re at an event and start to feel uneasy, it’s okay to leave early.
2. Family Conflict and Stress
For many, family relationships can be a source of both comfort and stress, especially during the holidays. Old family dynamics, unresolved conflicts, and emotionally charged interactions can quickly escalate and create stress, leading to powerful urges to relapse as a way to cope. Even positive family relationships may sometimes become overwhelming during this time of year.
To minimize the stress of family gatherings, establish clear boundaries before the event. Let family members know what topics of conversation are off-limits, and be prepared to walk away if tensions rise.
You don’t have to engage in every discussion, especially if it involves triggering topics. Practicing mindfulness or grounding exercises can help you stay calm in the moment, while breathing techniques can reduce immediate stress.
3. Loneliness and Isolation
Not everyone has a large or supportive family to spend the holidays with, and feelings of loneliness and isolation can be particularly intense during this season. Seeing others enjoy time with loved ones may make you feel disconnected, which can be a powerful trigger for relapse, especially if using substances was once a way to cope with loneliness.
One of the best ways to combat loneliness during the holidays is by staying connected with your recovery community. Many support groups, including Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), host additional meetings during the holidays to provide extra support.
Attending these meetings or reaching out to fellow group members can help you stay engaged and remind you that you’re not alone.
4. Financial Stress
The holidays can be an expensive time of year. Between buying gifts, traveling, and hosting celebrations, financial stress is a common issue that can lead to anxiety and potential relapse. Worrying about money might trigger old habits of using substances to escape feelings of overwhelm or inadequacy.
To manage financial stress, create a realistic budget for the holiday season. Remember that you don’t need to spend a lot of money to show appreciation for your loved ones. Homemade gifts, personalized cards, or simply spending quality time together can be just as meaningful as store-bought presents.
It’s also important to communicate with your family and friends if you’re unable to participate in expensive traditions. Most people will understand and appreciate your honesty.
5. Disruption of Routine

During the holiday season, your normal daily routine can be disrupted by travel, family visits, and social obligations. The lack of structure during the holiday season can lead to feelings of instability or chaos, making it harder to stay focused on recovery.
Regular routines, such as attending therapy sessions, going to recovery meetings, or practicing self-care, might not happen during the holidays, leading to increased vulnerability to relapse.
Even during the busy holiday season, try to maintain as much of your routine as possible. If you normally attend a support group meeting on a certain day, make it a priority, even if it means finding a meeting in a different location or attending virtually.
Plan out your schedule in advance so you know when and where you’ll be participating in recovery activities. Maintaining healthy habits like exercising, eating well, and getting enough sleep can also help you feel more grounded during this chaotic time.
6. Overconfidence in Recovery
Feeling confident in your recovery progress is a good thing, but overconfidence can sometimes lead to risky behavior. During the holiday season, this might mean attending parties where substances are present, thinking that you can handle being around them without temptation.
Overconfidence can also cause some people to stop attending support groups or neglect other recovery practices, believing they no longer need them.
While it’s wonderful to feel strong in your recovery, it’s important to stay humble and recognize that recovery is a lifelong process. Remind yourself that triggers can appear when you least expect them and maintaining healthy boundaries is essential for long-term sobriety. Keep attending support group meetings or talking to a sponsor regularly, even if you feel like you’re doing well.
7. Negative Emotions and Seasonal Affective Disorder (SAD)
The holiday season occurs during a time of year when shorter days and colder weather can lead to seasonal affective disorder (SAD) or feelings of sadness and depression. For those already managing mental health challenges, these seasonal factors can exacerbate negative emotions, increasing the temptation to relapse.
If you know you are prone to SAD or feelings of depression during the winter months, take proactive steps to care for your mental health. Light therapy, getting outside in natural daylight, and staying physically active are all proven methods for combating SAD.
Practicing mindfulness or engaging in creative activities like journaling, drawing, or music can help lift your mood. Understanding how to avoid relapse triggers related to emotional health is crucial for maintaining sobriety during this challenging season.
Find Strength and Avoid Relapse During the Holidays With Lumina Recovery
Relapsing during the holiday season can feel discouraging, but it’s important to remember that relapse is often part of the recovery journey. If you or a loved one experiences a relapse, don’t lose hope. Reach out for support immediately, whether that’s through a counselor, sponsor, or rehab facility.
At Lumina Recovery, we understand the challenges of maintaining sobriety during the holidays, and we’re here to help. If you’ve relapsed or are worried about holiday relapse triggers, our compassionate team offers evidence-based treatment plans that include coping strategies for triggers for relapse and ongoing support to get you back on the path to recovery.
If you’ve relapsed or are struggling with sobriety this holiday season, contact us today to get the support you need.

How to Support a Loved One With Depression
Knowing how to support someone with depression can be challenging. Depression is a complex mental health condition that affects how a person thinks, feels, and acts.
While it can be overwhelming to witness, knowing how to offer the right kind of support can make a significant difference in their journey toward recovery.
6 Ways to Support a Loved One With Depression
Here are some effective ways to offer support to a friend, family member, or loved one who is struggling with depression, helping them feel understood, cared for, and less alone in their journey.
1. Educate Yourself About Depression
Understanding what depression feels like and how it affects individuals can help you provide better support. Depression is not just a phase or something someone can “snap out of.” Learning about the condition can prevent you from making unhelpful comments, such as “just think positive” or “it’s all in your head.”
Take time to read about common treatment options for symptoms of depression, like therapy and medication, so you can offer informed suggestions if needed.
2. Encourage Open Communication
Talk to the person who is experiencing depression and let them know that you are there for them, no matter what. Encourage them to talk about how they’re feeling, and listen without judgment. Sometimes, just knowing that someone cares enough to listen can make a big difference.
Avoid pressuring them to talk if they are not ready. Respect their need for space, but remind them that you are available whenever they want to share.
3. Offer Practical Support
Depression can make even simple daily tasks feel overwhelming. Offering to help with routine activities, such as cooking meals, running errands, or tidying up, can relieve some of their burden.
Ask how you can help, rather than assuming what they need. Sometimes, small gestures like accompanying them to a doctor’s appointment or checking in with a text message can provide significant comfort.
4. Encourage Them to Seek Professional Help
People with depression often require treatment from mental health professionals. Encourage your loved one to consider therapy sessions, a counselor, or psychiatrist. Offer to help them research professionals or even go with them to their first appointment if they feel anxious.
Reassure them that seeking help is a sign of strength, not weakness. If they’re unsure about therapy, suggest starting with a simple consultation to see how they feel about it.
5. Be Patient and Compassionate
Recovery from depression takes time, and there may be days when your loved one seems to be doing better, followed by days when they seem to relapse. Be patient and compassionate throughout this journey.
Let them know that it’s okay to have bad days, and they are not alone. Remind them that recovery is not linear, and setbacks don’t mean they’re failing.
6. Encourage Healthy Habits
Depression often affects sleep, appetite, and activity levels. While it’s essential to be mindful not to push too hard, gently encourage your loved one to adopt healthy habits like regular sleep, social activities, balanced meals, and physical activity.
Suggest engaging in activities that promote relaxation, such as yoga, meditation, or spending time in nature. You could even offer to join them, turning it into an opportunity to bond.
4 Signs That Depression May Be Leading to Substance Abuse
Depression can be incredibly painful, and some individuals may turn to substances as a way to cope with their overwhelming feelings. Here are some signs that your loved one may be using drugs or alcohol to deal with their depression:
1. Increased Secrecy or Isolation
If your loved one has started avoiding friends, family, or social events more than usual, it could be a sign of deeper struggles. They might be using substances in isolation to numb their emotions.
2. Changes in Physical Appearance or Behavior
Noticeable weight loss or gain, bloodshot eyes, or a lack of personal hygiene can be indications of substance use. Behavioral changes like agitation, mood swings, or appearing excessively tired can also be red flags.
If they are struggling to maintain their responsibilities at work, school, or home, this could indicate a problem that requires attention.
3. Frequent Use of Alcohol or Drugs
Pay attention to whether your loved one is using alcohol or drugs more frequently or in larger quantities. Statements like, “I need a drink to relax” or “I can’t sleep without taking something” may be attempts to self-medicate.
Watch for substances being used as a crutch to get through daily activities or as a way to cope with difficult emotions.
4. Financial Issues or Legal Trouble
Unexplained financial issues, such as frequent borrowing of money, selling possessions, or financial secrecy, could suggest substance abuse. Legal trouble, such as driving under the influence or arrests related to drug possession, is a clear sign that they need help.

How to Talk About Seeking Help for Both Depression and Addiction
If you notice a loved one showing symptoms of depression and substance abuse, approaching the topic with sensitivity is crucial. Here are some tips:
Choose a Good Place and Time
Pick a quiet, private time when you can talk without intrusions. Ensure both of you are calm, and approach the conversation with empathy and care.
Avoid discussing this when either of you is feeling emotional or distracted, as this can lead to defensive reactions.
Express Your Concerns Without Judgment
Use “I” statements to communicate your worries. For example, say, “I’ve noticed that you seem very down lately, and I’m concerned about how much you’ve been drinking. I want to help you because I care.”
Avoid accusations or blaming, which can cause them to shut down. Instead, emphasize that you can support them, not to criticize.
Offer to Help Them Find Support
Research treatment options, such as integrated therapy for co-occurring disorders, which addresses both depression and substance abuse. Offer to help them find resources, whether that’s providing information on local treatment centers, support groups, or supporting them in making an appointment.
Encourage them to reach out to professionals who specialize in treating co-occurring disorders, as this approach provides a more holistic solution to their struggles.
Respect Their Autonomy But Encourage Action
While you cannot force someone to seek help, you can gently remind them of the benefits of seeking treatment. Respect their decisions, but don’t give up on offering support. Sometimes, planting the seed can lead to them taking action later on.
Remind them that they do not have to face depression and addiction alone. Let them know that seeking help is a brave step toward healing.
Guide Your Loved One Toward Healing With Lumina Recovery
Supporting a loved one who experiences depression is not always easy, especially if they are also using addiction as a way to cope. By educating yourself, offering practical support, and approaching difficult conversations with empathy, you can play a significant role in their journey toward recovery. Encourage them to seek professional help for both depression and substance use, and remind them that there is hope for a better future.
Lumina Recovery offers holistic dual diagnosis support and therapy services that address both depression and addiction, helping individuals find healing from both conditions simultaneously.
If your loved one is struggling with both depression and addiction, reach out to Lumina Recovery today for compassionate, expert care.

The Link Between Rumination and Substance Abuse
Many people face moments of overthinking and stress, but when these moments become persistent, they can evolve into rumination—a repetitive cycle of negative thinking that is hard to escape.
This constant mental replay of distressing thoughts can lead to significant mental health issues, and in some cases, it can drive individuals to use substances as a way to cope. Understanding the link between rumination and substance abuse is essential for those struggling with addiction or for concerned loved ones trying to support someone in recovery.
What Is Rumination?
Rumination is a mental habit where a person continuously dwells on negative thoughts or past events, replaying them over and over in their mind. According to the rumination definition in mental health, this pattern of overthinking often includes intrusive and repetitive thoughts that can lead to heightened anxiety, depression, and a sense of hopelessness.
When a person is stuck in this cycle, it becomes difficult to focus on anything positive, and they may find themselves feeling overwhelmed.
What Is the Link Between Rumination and Substance Abuse?
Substance abuse can be a way for individuals to escape from the mental distress caused by rumination. When someone is trapped in a loop of negative thinking, they might turn to alcohol, drugs, or other substances as a way to numb the pain.
For example, someone who is constantly thinking about a traumatic event or their perceived failures may use alcohol to temporarily forget these thoughts, or they may take drugs to feel a sense of relief from their persistent anxiety.
This is where the connection between substance abuse, ruminations, and intrusive thoughts becomes clear. When negative thoughts become intrusive, making it difficult for someone to function normally, self-medication may appear to be an accessible solution. Unfortunately, while substances might offer short-term relief, they often exacerbate the problem in the long run, leading to a dangerous cycle of dependence and addiction.
Rumination as a Risk Factor for Addiction
People who tend to ruminate may also be more susceptible to addiction. When someone habitually engages in repetitive negative thinking, they are more likely to feel depressed or anxious, both of which are common triggers for substance abuse.
Rumination can intensify feelings of distress, leading to a higher likelihood of turning to substances as a coping mechanism. For instance, if a person is unable to stop replaying a painful memory, they may seek out substances to block those thoughts or feelings, even if only for a moment.
Moreover, rumination can lead to a decreased ability to cope with stress. When a person’s mind is preoccupied with negative thoughts, it can be challenging to see solutions to their problems or to engage in healthy coping strategies. This lack of coping skills can drive someone to use drugs or alcohol to manage their emotions, setting the stage for addiction to develop.
Rumination During the Recovery Process
While rumination is a risk factor for the onset of addiction, it can also pose challenges during the recovery process. For many people in recovery, confronting the underlying reasons behind their substance use is a crucial step.
However, this confrontation can sometimes trigger intrusive rumination—the persistent rethinking of past mistakes, regrets, or the impacts of their addiction on themselves and others. If not managed properly, these thoughts can lead to relapse, as the individual might turn to substances to escape their guilt or shame.
During recovery, learning how to deal with intrusive rumination is essential. If someone is consistently focused on their past failures, they may struggle to believe in their ability to maintain sobriety, leading to a sense of hopelessness that fuels the desire to use again.
Recovery programs that include cognitive behavioral therapy (CBT) can be effective because they help individuals identify and change negative thought patterns, reducing the power of rumination.

5 Ways to Break the Cycle of Rumination
Breaking free from the cycle of rumination requires awareness and deliberate effort. Here are some strategies that can help:
- Mindfulness and Meditation: Practicing mindfulness can be a powerful tool in combating rumination. By focusing on the present moment rather than dwelling on past events, individuals can interrupt the cycle of repetitive negative thinking. Mindfulness exercises, like deep breathing and guided meditation, can also provide relaxation, which helps to manage stress and anxiety.
- Cognitive Behavioral Therapy (CBT): CBT is a therapeutic approach that helps individuals understand how their thoughts influence their emotions and behaviors. By identifying irrational or unhelpful thoughts, people can learn to challenge them and replace them with more positive, constructive thoughts. CBT can offer a way to address the root cause of their substance use, including their tendency to ruminate.
- Engaging in Activities: Keeping busy with activities that are fulfilling can redirect attention away from negative thoughts. Whether it’s picking up a new hobby, engaging in physical exercise, or spending time with loved ones, staying active can prevent the mind from becoming overwhelmed by ruminative thoughts.
- Seeking Professional Help: If someone finds that rumination is leading them toward substance use or affecting their recovery, it’s essential to seek professional help. Therapy can provide guidance on how to manage intrusive thoughts, and support groups can offer a sense of community and understanding from others who are experiencing similar struggles.
- Journaling: Writing down thoughts and emotions can be a therapeutic way to process feelings without them taking over the mind. Journaling allows individuals to explore their thoughts and release them onto paper, helping to break the cycle of rumination.
Empower Your Recovery Journey With Lumina Recovery
Rumination is more than just overthinking—it’s a relentless cycle of negative thoughts that can lead to severe mental health issues and increase the risk of substance abuse. Whether someone is just starting their recovery journey or is struggling to maintain sobriety, learning to manage intrusive rumination can be a key part of their success.
At Lumina Recovery, we offer a range of therapy services and dual diagnosis programs, designed to help individuals address underlying issues like rumination that contribute to substance abuse, fostering healthier coping strategies for long-term recovery.
Contact us today to learn how our personalized treatment programs can support you in overcoming addiction and breaking the cycle of rumination.

Using HALT to Identify Relapse Triggers in Recovery
Recovery from a substance use disorder is a challenging journey that requires constant vigilance and self-awareness. One of the most critical aspects of maintaining sobriety is recognizing and managing emotional triggers. Among the many tools available, the HALT method stands out for its simplicity and effectiveness.
HALT is an acronym that reminds individuals in recovery to prevent relapse by checking in with themselves and addressing four key areas: hunger, anger, loneliness, and tiredness. By learning to identify and manage these states, people can significantly reduce the risk of relapse and continue to thrive in their recovery journey.
What Is HALT?
HALT stands for hungry, angry, lonely, and tired—four physical and emotional states that can make a person more vulnerable to relapse. Each of these feelings, when unaddressed, can be a common trigger, increasing the likelihood of turning back to substances for comfort or relief. By understanding and addressing each of these states, individuals can build resilience against relapse.
H – Hungry
Hunger goes beyond just the physical need for food. While maintaining a balanced diet, regular meals, and healthy snacks are essential, hunger can also represent a craving for other forms of nourishment, such as emotional support, affection, or a sense of purpose.
Ignoring physical hunger and skipping meals can lead to a drop in blood sugar, causing irritability and poor decision-making, making it easier for addictive behaviors to resurface. It’s equally important to be mindful of emotional hunger.
Feeling deprived of love, comfort, or support can drive someone to seek out substances as a way to fill that void. Therefore, staying physically and emotionally nourished helps maintain balance and prevents vulnerability to relapse.
A – Angry
Anger is a powerful emotion that, if left unchecked, can quickly lead to relapse. Many people turn to substances as a way to numb or escape from the intensity of their emotions. In recovery, learning to process and express anger healthily is crucial.
This might involve strategies such as mindfulness, breathing exercises, or speaking with a therapist. Recognizing when anger is surfacing allows individuals to take proactive steps to manage it, rather than letting it build up to the point where it threatens sobriety. Taking a pause to address anger constructively can defuse its potential as a relapse trigger.
L – Lonely
Loneliness can be one of the most challenging feelings to deal with during recovery. Isolation often plays a significant role in addiction, and many people struggle to reconnect with others after starting their sobriety journey. Recovery requires a supportive community, whether it’s through family, friends, or a support group.
Feeling isolated can lead to seeking comfort in substances, so it’s important to recognize the signs of loneliness and take steps to engage with others. Reaching out for support, joining recovery groups, or finding activities that involve social interaction can help counteract feelings of loneliness and foster a sense of belonging.
T – Tired
Tiredness, both physical and mental, can deplete one’s ability to cope with stress and make healthy choices. When someone is exhausted, they are less likely to be mindful of their emotions, less resilient to cravings, and more inclined to make impulsive decisions, including reaching for substances.
Ensuring a good night’s sleep, establishing a regular sleep routine, and taking breaks when needed are all essential for maintaining stability in recovery. Mental fatigue should also be addressed—taking on too much at once can lead to burnout. Learning to pace oneself and set realistic goals can help maintain energy levels and keep stress in check.
How HALT Helps in Addiction Recovery
The concept of HALT is simple yet effective. It serves as a quick and easy way to self-check whenever cravings or difficult emotions arise. By regularly asking themselves, “Am I feeling hungry, angry, lonely, or tired?” individuals can better understand their triggers and take steps to address them before they escalate into a craving or a relapse situation.
For example, if someone recognizes that they are feeling lonely, they might call a friend, attend a support group meeting, or engage in an activity that brings them joy. Similarly, if they realize they are tired, they can make time for rest or adjust their schedule to avoid overexertion.

Practical Tips for Using HALT
Here are some practical tips for incorporating the HALT method into your daily routine to help manage and reduce relapse triggers during recovery.
- Keep a journal. Journaling can be a powerful way to monitor and understand your emotional and physical states. Each day, take a few minutes to write down how you’re feeling, noting any moments when you experienced hunger, anger, loneliness, or tiredness. Over time, this practice can help you identify patterns and triggers, making it easier to address them before they become overwhelming.
- Create a support network. It’s important to have a list of people you can turn to when you feel vulnerable. This network could include friends, family members, therapists, or members of a recovery support group. Knowing who you can call when you’re feeling lonely or angry provides a safety net, so you don’t have to face difficult emotions on your own.
- Develop healthy coping mechanisms. Each aspect of HALT can be addressed with proactive coping strategies. For example, keep snacks handy to prevent hunger, practice mindfulness or exercise to manage anger, join clubs or attend meetings to combat loneliness, and establish a consistent sleep routine to avoid tiredness.
- Set reminders. Life can get busy, and it’s easy to overlook your needs. Setting reminders on your phone to periodically check in with yourself can help maintain awareness. These reminders can be simple questions like, “How am I feeling right now?” or “Do I need a break?” A few moments of self-reflection throughout the day can make a big difference in managing emotions.
- Practice self-compassion. Recovery isn’t about perfection—it’s about progress. Be kind to yourself when you experience setbacks or find yourself struggling with HALT triggers. Acknowledge that it’s okay to have difficult days and that each challenge offers an opportunity for growth.
Stay Resilient in Recovery With Lumina Recovery
The HALT method is a valuable tool for anyone in recovery because it simplifies the complex process of self-awareness into four manageable categories. By regularly checking in on whether they are hungry, angry, lonely, or tired, individuals can address their needs before they lead to potentially risky behavior.
Lumina Recovery offers a range of therapy services and specialized rehab programs designed to help individuals understand and manage triggers, like those addressed in the HALT method, to support long-term recovery success.
If you or a loved one needs support on your recovery journey, contact Lumina Recovery today for compassionate and personalized care.

Understanding Panic Disorder and Its Connection to Addiction
Panic disorder is a condition that can severely disrupt a person’s life. People with panic disorder experience sudden, intense episodes of fear that can feel overwhelming and debilitating.
For someone struggling with panic disorder, the search for relief from this intense anxiety can sometimes lead to a substance use disorder or addiction as a coping mechanism. Understanding the connection between panic disorder and addiction is vital for those seeking to break free from both challenges.
What Is Panic Disorder?
Panic disorder is a type of anxiety disorder that causes frequent and unexpected panic attacks. Experiencing at least two panic attacks can lead to a diagnosis of panic disorder.1
These attacks often come without warning and can mimic life-threatening situations, leaving individuals feeling anxiety symptoms and uncertain of when the next one might strike. People may experience panic attacks that last between 5 and 10 minutes but may linger for hours.
People with panic disorder may begin to live in fear of their next attack, avoiding places or situations they believe might trigger one. This can lead to social isolation and a reduced quality of life, as everyday tasks become sources of anxiety. For many, this chronic stress creates a constant search for relief, which may include turning to substances like alcohol or drugs.
Symptoms of Panic Disorder
Panic attack symptoms vary from person to person but may include some of the following:1
- A sense of impending danger
- Sweating
- Trembling or shaking
- Shortness of breath
- Throat tightness
- Abdominal cramps
- Headaches
- A choking sensation
These symptoms can feel terrifying, and because they often occur without warning, the uncertainty adds another layer of distress to a person’s life.
Triggers of Panic Disorder
Certain factors can increase the likelihood of developing panic disorder, though the exact causes are not always clear. Some of the most common triggers include:1
- Family history: If someone in your family has panic disorder, you may be at an increased risk of developing it. It’s unclear whether this is due to genetics or the environment you grew up in.
- High levels of stress: Stressful events or prolonged exposure to stress can trigger panic attacks and lead to the development of panic disorder.
- Difficulty handling negative emotions: People who frequently experience negative feelings or have trouble coping with emotions are more vulnerable to panic attacks.
In addition to these factors, there are other conditions and habits that are believed to put those at high risk for panic disorder:1
- Depression: Many people with panic disorder also struggle with mental health conditions like depression, which can increase the frequency and intensity of panic attacks.
- Alcohol abuse: Drinking alcohol excessively can contribute to the development of panic disorder.
- Cigarette smoking: Smoking is linked to both anxiety and panic
- Suicide risk: Individuals with panic disorder may face a higher risk of suicidal thoughts, especially when combined with other mental health challenges.
- Seasonal affective disorder (SAD): This type of depression, which typically occurs during the winter months, may also be linked to increased anxiety and panic
How Panic Disorder Can Lead to Addiction
For individuals with panic disorder, the constant fear and unpredictability of panic attacks can feel overwhelming. Many turn to substances like alcohol, benzodiazepines, or other drugs as a way to numb the debilitating anxiety and regain a sense of control.
Initially, these substances may seem to provide temporary relief from the intense fear and tension that panic disorder brings. However, this relief is short-lived and often leads to long-term consequences.
There is a high substance use prevalence among panic disorder sufferers, as many individuals use substances to cope with overwhelming feelings. Over time, using substances as a coping mechanism can result in dependence, where the brain and body require these substances to function normally.
What begins as a way to escape panic attacks can evolve into a harmful cycle of addiction. The more frequently substances are used, the more tolerance builds, requiring higher doses to achieve the same effect. This often leads individuals to increase their consumption or turn to stronger drugs, further complicating their battle with both panic disorder and substance abuse.
Anxiety is one of the most common reasons people turn to substances, especially when coping with panic disorder. While drugs and alcohol may temporarily dull the emotional and physical symptoms of anxiety, they can ultimately worsen the condition. This creates a dangerous feedback loop: the substances intensify anxiety over time, leading to increased reliance on them, perpetuating both the panic disorder and the addiction.

Breaking the Cycle: Addressing Panic Disorder and Addiction
Recovery from both panic disorder and addiction is challenging, but seeking treatment can make recovery possible. A holistic treatment plan often requires a dual approach that addresses both the anxiety disorder and the substance use problem.
1. Therapy
Cognitive behavioral therapy (CBT) is one of the most effective treatments for panic disorder. It helps individuals understand their thought patterns and learn healthier ways to cope with anxiety. CBT can also help those struggling with addiction by addressing the underlying emotional triggers for their substance use.
2. Medication
Some individuals may benefit from medication to manage panic disorder. Antidepressants or non-addictive anti-anxiety medications can help control symptoms, without the risk of developing a new addiction.
3. Support Groups
Whether it’s a 12-step program or a support group for people with anxiety, having a network of people who understand the struggle can make a huge difference. Support groups provide a safe space to share experiences and learn from others.
4. Healthy Coping Mechanisms
Learning new ways to cope with anxiety is essential. Mindfulness, meditation, exercise, and other stress-reduction techniques can provide healthier alternatives to substance use when dealing with panic disorder.
Find the Support You Need for Panic Disorder and Addiction With Lumina Recovery
The connection between panic disorder and addiction is clear: both are powerful and often co-occurring challenges that feed into each other. Understanding the symptoms and triggers of panic disorder is essential in preventing the cycle of addiction from taking root. With the right treatment and support, individuals can learn to manage both their anxiety and substance use, leading to a healthier and more stable life.
Lumina Recovery offers dual diagnosis programs that address both anxiety and post-traumatic stress disorder (PTSD), providing specialized care for individuals whose panic disorder and related conditions contribute to substance use, ensuring a holistic path to recovery.
If you or a loved one is struggling with panic disorder and addiction, reach out to Lumina Recovery for professional support today.
Source:

The Link Between Phobias and Addiction
Phobias can be overwhelming and life-altering. When faced with intense and irrational fears, some people turn to harmful coping mechanisms like substance use. This can lead to a dangerous cycle in which the need to escape the fear leads to addiction. Understanding the connection between phobias and addiction is crucial to effectively addressing both issues.
What Is a Phobia?
A phobia is an irrational and excessive fear of an object, situation, or activity. While everyone experiences fear at times, phobias are marked by an overwhelming sense of dread or anxiety that can interfere with daily life.
Common phobias include fear of heights (acrophobia), fear of small spaces (claustrophobia), and fear of social interactions (social phobia). These intense reactions often seem out of proportion to the actual danger involved.1
For those suffering from phobias, daily tasks can feel unbearable. The fight-or-flight response, a biological reaction to danger, is triggered unnecessarily, leading to physical symptoms like sweating, trembling, and heart palpitations.1
These symptoms can be so distressing that individuals may go to great lengths to avoid the trigger, which significantly impacts their quality of life.
The Dangers of Self-Medication
Phobias can create overwhelming emotional and physical reactions. People struggling with these feelings may look for relief by self-medicating with drugs or alcohol. The temporary numbing effects of these substances may seem like a solution, but this only exacerbates the problem.
Self-medication involves using substances to cope with symptoms of mental health conditions like phobias. Over time, this behavior can lead to dependence, as individuals become addicted to the fleeting sense of relief the substances provide.
While the fear might be dulled temporarily, the root cause of the phobia remains untreated, and now the person is at risk of developing a substance use disorder.
One of the most concerning aspects of this behavior is that self-medication can quickly spiral into addiction. Many drugs and alcohol affect the brain’s reward system, releasing chemicals like dopamine that create feelings of pleasure.
As this cycle continues, individuals may find that they are not just escaping fear but becoming addicted to the substances themselves. This is where the link between phobias and addictions becomes more apparent.
The Connection Between Phobias and Addiction
The connection between phobias and addictions can be complex, with both conditions feeding into each other. People with severe phobias are often at higher risk of turning to substance use as a means of coping.
Addiction, in turn, can exacerbate the symptoms of phobias. For example, someone who develops a substance use disorder may begin to fear withdrawal symptoms or become isolated due to their addiction, which can worsen their phobic reactions.
Additionally, fear and addiction share a neurological connection. Both fear and pleasure are processed in the brain, and when someone is repeatedly exposed to a fearful situation, their brain may seek out ways to reduce the stress.
Addictive substances can offer temporary relief, tricking the brain into thinking it has found a way to cope with the fear. This can create a dangerous loop where the individual becomes not only afraid of their phobia but also addicted to fear itself, as their body constantly craves the relief that substances provide.
In this context, fear is no longer just a response to a specific situation but an ongoing state that drives addiction. It’s important to recognize that while the substances may seem to offer a way to escape, they are actually compounding the problem and making recovery more difficult.
Breaking the Cycle
Recognizing the dangerous relationship between phobias and addiction is a crucial step toward healing. Breaking this cycle requires a holistic treatment approach that addresses both the phobia and the addiction.
1. Addressing the Phobia
The first step in treating phobias is identifying the specific fear and understanding its root causes. Cognitive behavioral therapy (CBT) is one of the most effective treatments for phobias. This therapy focuses on changing thought patterns and behaviors that reinforce the fear.
For instance, someone with social phobia may work with a therapist to gradually expose themselves to social situations in a controlled, supportive environment. This is known as exposure therapy, a subset of CBT that helps reduce fear responses over time.
Exposure therapy works by helping individuals confront their fears in small, manageable steps. Over time, repeated exposure to the fear-inducing situation decreases anxiety and desensitizes the person to their fear. This method empowers individuals to regain control of their lives, reducing their reliance on harmful coping mechanisms like substance use.

2. Treating the Addiction
Treating the addiction side of the equation requires addressing both the physical and psychological dependence on substances.
Detoxification, often the first step in treatment, allows the body to rid itself of harmful substances under medical supervision. After detox, ongoing therapy is essential to address the root causes of addiction and develop healthier coping strategies.
Addiction treatment programs often incorporate behavioral therapies, like CBT or dialectical behavior therapy (DBT), to teach individuals how to manage stress, avoid relapse triggers, and replace unhealthy behaviors with positive habits.
Support groups, such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), can also provide individuals with a sense of community and accountability.
3. Receiving Dual Diagnosis Treatment
For individuals struggling with both phobias and addictions, dual diagnosis treatment is vital.
This integrated approach treats both conditions at the same time, rather than treating them as separate issues. Dual diagnosis programs provide a more comprehensive path to recovery by addressing the interplay between phobia-induced fear and substance use.
By treating both phobias and addictions simultaneously, individuals are more likely to achieve lasting recovery and break free from the cycle of fear and addiction.
Overcome Phobias and Addiction With Lumina Recovery
Phobias can significantly disrupt a person’s life, often leading to dangerous coping strategies like substance use. The link between phobias and addictions lies in the need to escape overwhelming fear, but self-medication only serves to deepen the cycle of addiction and anxiety. By understanding this connection and seeking proper treatment, individuals can break free from the grip of both phobias and addiction.
Lumina Recovery offers dual diagnosis programs for various addiction types, including alcohol, opioids, and prescription drugs, addressing both the addiction and phobias to ensure a holistic path to healing.
If you or a loved one is struggling with fear and addiction, reach out for expert care to guide you through recovery with Lumina Recovery.
Source:
What Is Chronic Stress and How Does It Affect You?
Stress has become a common part of life in our world today. While short-term stress can push you to meet deadlines or solve problems, chronic stress is a different story. When stress becomes long-lasting, it impacts every aspect of your life, causing physical, emotional, and mental challenges.
For individuals with addiction, chronic stress is especially concerning because it can contribute to both the development and worsening of substance use disorders. We will explore what chronic stress is, how it affects the body and mind, and its connection to addiction.
Chronic Stress Defined
Chronic stress is a type of stress characterized by prolonged emotional and physical tension, caused by ongoing pressures that feel overwhelming or unavoidable.
Unlike acute stress, which is brief and usually subsides once the immediate challenge or stressful situation has passed, chronic stress lingers and continues over an extended period. Common causes of chronic stress include work pressure, financial difficulties, relationship problems, and health concerns.
While occasional stress can actually improve performance, chronic stress keeps you in a constant state of alertness, leading to long-term strain on your body and mind. It activates the “fight-or-flight” response continuously and the body releases stress hormones such as cortisol and adrenaline.
The Physical Toll of Chronic Stress
When stress becomes chronic, your body can suffer a wide range of physical health problems. Symptoms of chronic stress include:1
- Heart Problems: Chronic stress can increase your risk of heart disease due to high blood pressure and cholesterol levels. It also contributes to an irregular heartbeat and increased risk of heart attacks.
- Weakened Immune System: Ongoing stress weakens your immune system, increasing your vulnerability to infections and illnesses. It can also slow the healing process when you’re sick or injured.
- Gastrointestinal Issues: Stress is known to affect digestion, leading to problems such as ulcers, irritable bowel syndrome (IBS), and chronic indigestion.
- Muscle Tension and Pain: Prolonged stress causes muscle tension, leading to headaches, back pain, and discomfort.
- Sleep Disturbances: Stress often leads to difficulty sleeping, including insomnia. Over time, poor sleep habits can further exacerbate stress, creating a vicious cycle.
The Emotional Toll of Chronic Stress
Beyond physical effects, chronic stress takes a significant toll on emotional and mental health. The emotional consequences for those who experience chronic stress can be just as harmful, contributing to:1
- Anxiety and Depression: Chronic stress is a well-known trigger for both anxiety and depression. The overwhelming nature of stress can make it difficult to relax or enjoy activities you once found pleasurable.
- Cognitive Decline: Stress impairs cognitive functions like memory, concentration, and decision-making. The longer you remain in a stressed state, the harder it becomes to focus on tasks or think clearly.
- Emotional Exhaustion: Chronic stress often leads to feelings of being emotionally drained or burned out, making it hard to cope with everyday challenges.
- Relationship Struggles: Constant stress can lead to irritability and mood swings, which can strain relationships with family members, friends, and coworkers.
Chronic Stress and Addiction
The connection between chronic stress and addiction is well-established. For many people, stress becomes a trigger that leads to substance use or other addictive behaviors.
People experiencing chronic stress may turn to drugs or alcohol as a way to cope with their overwhelming emotions. Substances can temporarily provide relief by numbing negative feelings, but this often leads to dependency and addiction over time.
Long-term stress affects the brain’s ability to regulate its response to stressors. As a result, individuals may seek out substances to escape or dull the persistent feelings of anxiety and tension caused by stress.
For individuals in recovery from addiction, chronic stress can be a significant factor that leads to relapse. The stress-induced craving for substances may overwhelm even the most well-intentioned efforts to stay sober.
Those who have a history of trauma, anxiety, or depression are often more vulnerable to chronic stress, which can then increase the likelihood of developing an addiction.

Managing Chronic Stress to Support Addiction Recovery
Addressing chronic stress is crucial in supporting long-term recovery. Here are some strategies to manage chronic stress effectively:
- Adopt healthy coping mechanisms. Developing healthy outlets for stress management such as regular physical activity, practicing mindfulness, or engaging in hobbies can help alleviate the effects of chronic stress.
- Try therapy and counseling. Cognitive behavioral therapy (CBT) and other forms of counseling are helpful for learning how to manage stress more effectively. Therapy can provide tools to reduce the emotional and mental burden of chronic stress.
- Build a support network. Connecting with others who understand your struggles, whether through support groups, family, or friends, can help relieve feelings of isolation that chronic stress often brings.
- Make lifestyle adjustments. Improving your diet, getting enough sleep, and reducing caffeine or alcohol intake can make a big difference in managing stress levels. Small, positive lifestyle changes can reduce the physical impact of stress on your body.
- Seek professional help. If chronic stress has contributed to addiction, professional treatment is often the best path forward. Addiction recovery programs can address both the underlying stress and the addiction itself, giving individuals the tools they need to recover and live healthier lives.
Find Support for Chronic Stress and Addiction With Lumina Recovery
Chronic stress can have serious consequences on your physical, emotional, and mental well-being. Left unmanaged, it can lead to or exacerbate addiction. However, by recognizing the signs of chronic stress and taking steps to address it, you can protect your health and work toward a more balanced, fulfilling life.
Lumina Recovery’s dual diagnosis services provide holistic care for individuals struggling with both addiction and chronic stress. By addressing the underlying mental health challenges that fuel substance use, these services support long-term recovery.
If you or a loved one is struggling with addiction and chronic stress, contact Lumina Recovery to help pave the way to a healthier, brighter future.
Source:

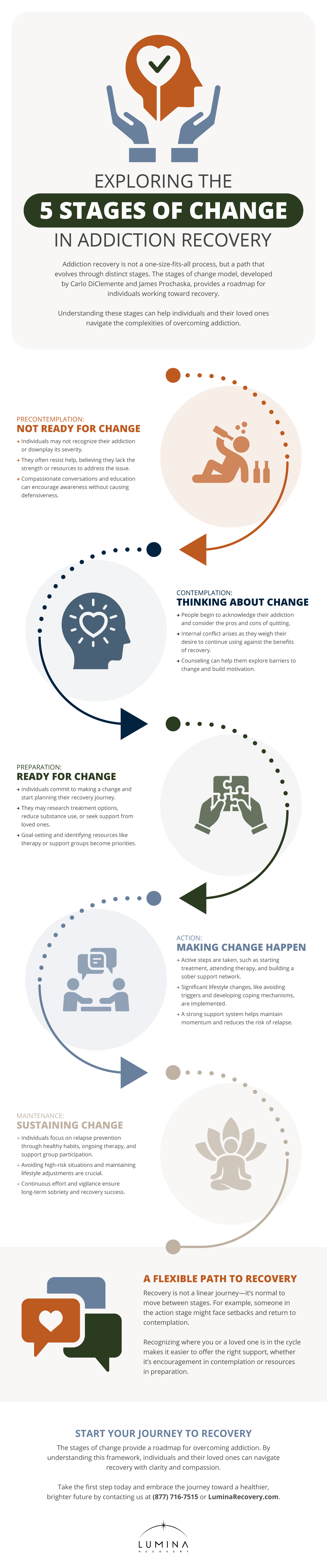
Exploring the 5 Stages of Change in Addiction Recovery
Addiction recovery is a journey that takes time, effort, and a deep commitment to change. One of the most widely recognized models that explains how individuals navigate the recovery journey is the stages of change model, also referred to as the transtheoretical model (TTM).
Created by psychologists Carlo DiClemente and James Prochaska, this model outlines five key stages that people go through when making significant changes in their lives, such as overcoming addiction. These stages include precontemplation, contemplation, preparation, action, and maintenance.1
Understanding where you or a loved one falls within these stages can provide insight into the recovery process and help frame expectations.
1. Precontemplation: Not Ready for Change
In the precontemplation stage, individuals are often unaware of their addiction to alcohol or drugs, or they may not fully recognize the severity of their problem. They may downplay the consequences of their substance use, feeling that it’s not yet an issue they need to address. Others in this stage may be aware of the risks but feel resistant to change because they do not believe they have the strength or resources to tackle their addiction.
In addiction recovery, people in this stage can have a particularly challenging time. Loved ones may notice the problem through their loved one’s addictive behaviors, but the individual in precontemplation might not be open to receiving help or taking steps toward recovery. It’s essential during this stage to approach the person with compassion and patience rather than judgment.
Staging an intervention, motivational conversations, or educating them about the dangers of addiction may help them progress to the next stage. However, pushing people with addictions too hard too soon can lead to further resistance.
2. Contemplation: Thinking About Change
In the contemplation stage, a person typically begins to recognize that their addiction is problematic. They may start to weigh the pros and cons of quitting or continuing their behavior. This internal struggle can be an emotional one, as people wrestle with their desire to keep using versus their desire to improve their health, relationships, and quality of life.
This is a crucial turning point in addiction recovery. While the person hasn’t committed to change yet, they are open to the idea that their life could be better without the addiction. During this stage, therapy and counseling can be highly beneficial in helping individuals explore their fears, doubts, and barriers to recovery.
3. Preparation: Ready for Change
The preparation stage is when an individual has made the decision to change. They may begin taking small steps toward recovery, such as cutting back on substance use or researching treatment options. At this point, they are no longer just thinking about recovery but preparing to take meaningful action.
This stage is where a person starts to map out a plan for their sobriety. Some individuals may begin to incorporate harm reduction strategies, seek advice from healthcare professionals, attend support group meetings, or tell friends and family about their decisions.
This is a critical time for setting realistic goals and identifying the right resources, whether that means entering an inpatient treatment center, starting outpatient therapy, or joining a 12-step program.
4. Action: Making Change Happen
In the action stage, the individual actively works on implementing the changes they have prepared for. This often includes entering an addiction treatment program, attending therapy sessions, and developing new coping mechanisms to deal with stress or triggers. The action stage requires significant commitment, as it often involves a complete lifestyle shift.
During this stage, the individual is immersed in the process of recovery. They may be detoxing from substances, undergoing counseling, and building a sober support network.
This stage is not only about adopting new behaviors and strategies that support long-term recovery—it’s also a time when relapse risk is higher, so having a structured support system is crucial. Encouragement and accountability from loved ones and professionals can help maintain their momentum.

5. Maintenance: Sustaining Change
The final stage is maintenance, where the individual has achieved sobriety and is focused on maintaining their progress. The main goal in this stage is to avoid relapse by continuing to practice healthy habits, attending support groups, and seeking help when needed. It’s important to recognize that maintenance is about staying vigilant and committed to long-term recovery.
In the maintenance stage, individuals are focused on staying sober and building a life that supports this commitment. This might include making significant lifestyle changes, such as avoiding environments that promote substance use or cutting ties with friends who still engage in those behaviors.
This stage also emphasizes the importance of ongoing therapy and the participation in aftercare programs. Relapse prevention strategies become vital, as staying on the path of recovery requires continuous effort.
The Stages of Change and Addiction Recovery
The stages of change model provides a helpful framework for understanding the process of addiction recovery. It emphasizes that recovery is not a linear journey but one that may involve moving between stages.
For instance, someone in the action stage may experience a setback and revert to contemplation or preparation. This is normal, and understanding the stage a person is in can help guide appropriate responses and support.
By recognizing where you or your loved one is in this cycle, it becomes easier to offer the right kind of support. Whether it’s encouraging them to think about the consequences of their addiction in the contemplation stage or helping them find the right resources during preparation, meeting them where they are can make a significant difference in their recovery journey.
Embrace Every Stage of Your Recovery Journey With Lumina Recovery
Recovery from addiction is a challenging, lifelong process that involves moving through various stages of change. Each stage brings its own set of challenges, but with the right support, individuals can progress toward a healthier, substance-free life. Understanding these stages not only provides clarity but also helps set realistic expectations for recovery.
Lumina Recovery offers dual diagnosis services and therapy programs that address both addiction and underlying mental health conditions, ensuring that individuals in each stage of recovery receive the tailored care they need to achieve lasting sobriety.
If you or someone you love is ready to take the next step toward lasting recovery, reach out to Lumina Recovery for compassionate support and guidance.
Source:
Additional Resources
Once you have completed your rehabilitation program at one of our drug and alcohol treatment centers, you should try to surround yourself with people who can encourage you to stay sober. Many people find that support groups are the best source of encouragement. You can find hundreds of support groups and meetings in your community. Our drug addiction treatment centers stress the importance of personal chemical dependency resources, especially when you are new to sobriety. Below are various addiction and mental health resources for people in recovery who want additional support.
Christian Addiction Recovery Resources
Our substance abuse services aren’t limited to specific programs, but rather we believe in the importance of incorporating faith-based programs to promote spiritual healing, like our Faith in Recovery program.
With that said, below are some faith-based addiction recovery resources that could help you in your spiritual healing from addiction:
- Battlefield of the Mind by Joyce Meyer
- Boundaries by Dr. Henry Cloud & Dr. John Townsend
- Christian Families in Recovery: A Guide for Addiction, Recovery, and Intervention Using God’s Tools of Redemption by Robert and Stephanie Tucker
- Club New Life Christian Ministry for Addiction and Recovery
- Lost & Found: Recovery in Christ by Bruce Stanley
- Overcoming Emotional Obstacles through Faith: Navigating the Mind Field by Anthony Acampora, Director of Banyan’s Faith in Recovery Program
- The Case for Christ by Lee Strobel
Mental Health Resources for Recovery
Lumina Recovery consist of both mental health and substance abuse treatment facilities, meaning we offer mental health resources as well as chemical dependency resources. What’s more, addiction often co-occurs with mental illness, making these resources ever more important.
Below are some resources for mental health recovery that can help you or your loved one:
- This Emotional Life video series
- No Kidding, Me 2!! with Joe Pantoliano
- Dare: The New Way to End Anxiety and Stop Panic Attacks by Barry McDonagh
- Pleasure Unwoven: An Explanation of the Brain Disease of Addiction by Kevin McCauley
- Declutter Your Mind: How to Stop Worrying, Relieve Anxiety, and Eliminate Negative Thinking by S.J. Scott and Barrie Davenport
Call Us Today – (877) 716-7515

