Our Addiction Resources
Navigating the world of addiction and recovery can be overwhelming. We’re here to provide clear, compassionate education and guidance. From practical advice for maintaining sobriety to informational guidance on the long-term effects of substance abuse, our content is a beacon of hope and understanding.
Our Team is Ready are ready to take your call
Call us Today!
or we can call you. Fill out form below
Our Blog

How to Build a Support System in Recovery
Addiction is a serious and life-threatening condition, and the path to sobriety is a lifelong journey. However, you don’t have to walk this path alone. There are people who care deeply about you and are ready to offer their support. Building a strong support system can make a world of difference—helping you avoid isolation and depression, reduce the risk of relapse, and ensure you have the encouragement and resources needed to thrive.
Let’s explore how you can create a support network that truly supports and uplifts you.
What Is a Recovery Support System?
A recovery support system is a network of people who offer emotional, practical, or spiritual support. These sources of support can be divided into two types: personal and recovery-focused.
Personal and social support systems might include:
- Family members and relatives
- Friends who support your sobriety
- Colleagues with shared recovery experiences
- Members of your faith or community groups
When evaluating your personal support, ask yourself if those around you are helping or hindering your recovery. You need individuals who uplift your self-esteem and help you avoid triggering situations. Be intentional about surrounding yourself with people you can genuinely trust.
Recovery support systems are tailored specifically for those in recovery and may include:
- 12-step programs
- Sober living environments
- Individual and group therapy
- Sponsors
- Medical professionals
Once you’ve chosen who you want in your support system, take the time to consider what you need from them. Clearly communicate these needs so they can support you effectively and in a way that feels right for both of you.
What Are the Benefits of a Recovery Support System?
People in your support system not only provide emotional and practical support but also play a crucial role in your overall success. Here’s how a supportive recovery network can positively impact your journey:
- Boosts Mental Health: Strong social connections can significantly improve mental health, reducing the risk of conditions like depression, anxiety, and PTSD, which can feel overwhelming during times of crisis. Feeling supported and understood can help you stay resilient and hopeful.
- Reduces Relapse Risk: A reliable support network is vital for preventing relapse. Establishing a regular check-in schedule with trusted friends, a sponsor, or a therapist creates a safety net and provides accountability and a sense of solidarity during difficult times.
- Enhances Treatment Engagement: When friends and family are cheering you on you feel loved and supported. When they are engaged, interested and follow up on your progress regularly this can inspire you to show up and see recovery as an exciting challenge—one you can accomplish—and not a chore.
- Improves Coping Skills: Social support can help reduce stress and enable coping with the ‘hard stuff’ that rears its head in recovery. Knowing you can reach out to people who relate to you and don’t judge you or give you flippant answers can help you manage difficult moments more effectively.
- Supports Physical Health: Friends or family who lead active lives can encourage you to join them in physical pursuits, which can help increase endorphin levels and give you a sense of achievement and the knowledge to realize how great you feel after exercise. This can be a great encouragement to stay sober.

How Do You Build a Recovery Support System?
Having a network of supportive, understanding individuals can make a significant difference in your journey. It’s not just about meeting new people in recovery to lean on when times are tough—it’s about creating connections that uplift you, keep you accountable, and provide a sense of community. Here’s a guide to help you build a strong, significant support network that will encourage and sustain you throughout your recovery.
Frequently attend 12-step meetings. Whether you choose AA, NA, or another 12-step program, attending meetings regularly—whether in person or online—offers a safe, supportive space where you can connect with others who truly understand your struggles. Over time, you may form lifelong friendships. As you continue in your recovery, keeping up with meetings helps you stay grounded and provides an opportunity to give back by supporting others on their journey.
Consider a sponsor. A peer sponsor, someone who has walked a similar path, can offer invaluable guidance and encouragement. They genuinely understand your experiences and can provide insightful support and accountability, helping you stay on track for years to come.
Get professional support. Working with a therapist, counselor, or recovery coach adds another layer of support. These professionals can help you address personal challenges, develop effective coping strategies, and stay on track with your recovery goals.
Find demographic-specific groups. Seek out support groups that cater to your specific needs, such as those for individuals with co-occurring conditions or particular mental health issues alongside addiction. These groups can offer more tailored support and a deeper understanding of your unique challenges.
Participate in service work. Engaging in service work within your recovery group or the broader community helps you connect with others dedicated to positive change. It also provides a sense of purpose and fulfillment, strengthening your own commitment to change.
Explore meet-up groups. Seek out meet-up groups with sober individuals who share your interests and hobbies—could be anything from book clubs to yoga sessions in the park. Connecting with like-minded people who enjoy similar activities can significantly boost your state of mind and foster a strong sense of camaraderie.
By taking these steps, you’ll cultivate a supportive network that not only aids your recovery but also enriches your life with meaningful connections and experiences.
Find Support at Lumina Recovery
At Lumina Recovery we are committed to helping you create an aftercare plan that ensures the highest chances of a sustained recovery. Our dedicated treatment team of professional therapists and counselors work closely with clients to create a recovery plan based on each individual’s specific needs.
From telehealth services to sober living options to an extensive alumni network, Lumina Recovery is here to help you stay on track with your recovery goals.
Contact us to learn more about how our integrated recovery options can be personalized to support your journey to wellness.

Starting a New College School Year While Sober
Starting a new college year can be exciting, but it can also present unique challenges, especially for students who are in recovery or committed to maintaining their sobriety. College environments often come with social pressures and stressors that can make staying sober difficult.
However, with the right strategies and support systems, you can not only survive but thrive while remaining sober. Below, we’ll provide guidance on navigating social pressures, managing academic and emotional stress, and finding sober support networks on campus.
Navigating Social Pressures
One of the biggest challenges of being sober in college is handling the social pressures of campus life. Parties, tailgating events, and social gatherings often involve alcohol or drugs. Here’s how to manage these situations:
1. Build a Sober Social Circle
Find friends who respect your sobriety or share your commitment to being substance-free. You don’t have to surround yourself with people who drink or use drugs. Seek out like-minded individuals who prioritize health and well-being. Many campuses offer recovery dorms or sober living options or arrangements, which can be a great way to connect with other students in recovery.
2. Be Prepared With Responses
When offered a drink or invited to a party, have a prepared response. A simple, “No thanks, I don’t drink, but I’d love to hang out,” can be enough. Having a prepared assertive yet polite answer ready can help you feel more confident in social settings.
3. Choose Social Events Wisely
You don’t need to attend every event. Be selective and attend events where alcohol and drugs aren’t the main focus. Many schools host sober college events like movie nights, fitness classes, or outdoor adventures. These activities offer a great way to have fun without the pressure to use substances.
4. Practice Assertiveness
Peer pressure can be intense in college, but it’s crucial to remain firm in your choices. If you find yourself in a situation where others are pressuring you, remember it’s okay to leave. Setting boundaries is important, and sticking to them will help you protect your sobriety.
Managing Stress Without Substances
College can be stressful, and for many students, substances were once a way to cope with that stress. However, there are healthier ways to manage stress while staying sober.
1. Establish a Daily Routine
Creating a daily routine can provide structure and reduce anxiety. Schedule regular times for studying, exercise, meals, and relaxation. A routine helps you stay organized and avoid last-minute stress, which could trigger cravings. Including self-care activities in your day, such as walking or journaling, is also important.
2. Practice Mindfulness
Mindfulness practices like meditation or deep breathing can help you stay grounded when stress levels rise. Taking just 10 minutes a day to meditate can make a big difference in your emotional health. Many campuses offer free or low-cost mindfulness workshops or yoga classes, which can be helpful tools in your stress management toolkit.
3. Exercise Regularly
Exercise releases endorphins, which naturally reduce stress and improve your mood. Whether it’s a run, gym workout, or yoga class, physical activity is a great way to handle stress. Regular exercise can also improve your sleep and boost energy, both of which are important for staying on track academically and emotionally.
4. Seek Academic Support
Academic stress can quickly become overwhelming, but colleges offer many resources to help. Tutors, writing centers, and study groups are valuable tools for staying on top of your coursework. If you’re feeling overwhelmed, talk to your professors or academic advisors. They may offer extensions or guidance on managing your workload.
5. Connect with Counseling Services
Most colleges offer mental health counseling services for students. Whether it’s one-on-one counseling or group therapy, these services can help you cope with the pressures of college life. Counselors can provide emotional support and practical strategies for managing stress without turning to substances.
Finding Sober Support Networks on Campus
A crucial part of being sober in college is finding the right support system. Having people around who understand and support your commitment to sobriety is key to your success. Fortunately, many colleges now offer resources for students who are either in recovery or want to stay sober during their academic journey.
1. Join a Sober Student Group
Many colleges have recovery or sober student groups, often sponsored by the health and wellness office. These groups provide a safe space for students who are committed to sobriety. They can be a great source of support, accountability, and friendship. Look for groups like “Students for Recovery” or “Sober College Life” organizations, which cater specifically to students who want to live a substance-free life.
2. Connect With Campus Counseling Services
If your college offers counseling or mental health services, take advantage of them. Addiction in college students is not uncommon, and counselors are there to help you navigate the challenges you may face. These services can provide individual counseling or connect you with group therapy sessions focused on addiction recovery or managing stress without substances.
4. Find a Sober Mentor
Having a mentor who is also sober can be incredibly helpful as you navigate the ups and downs of college life. A sober mentor could be a fellow student who has more experience in recovery or a faculty member who understands the challenges of staying sober. They can provide guidance, support, and motivation as you continue your sobriety journey.
5. Utilize Online Communities
If you don’t have a strong sober community on campus, consider joining online sober networks. Online forums, social media groups, or virtual meetings offer platforms where you can connect with others in recovery. These communities provide a safe space to share experiences, ask questions, and find support from those who understand what you’re going through.
Start Your College Journey Strong With Lumina Recovery
Starting a new school year sober in college may feel daunting, but it is entirely possible with the right strategies and support systems in place. Many students are committed to their sobriety, and with the right mindset and support, you can make the most of your college experience while staying true to your commitment to sobriety.
Lumina Recovery offers a specialized program designed to support college students struggling with alcohol or drug addiction, providing tailored treatment and recovery resources to help them maintain sobriety while achieving academic success.
Embrace this exciting chapter of your life while staying true to your sobriety and thriving on campus by reaching out to Lumina Recovery.

5 Emerging Drug Trends to Be Aware Of
As drug markets continue to evolve, new and emerging drugs are becoming more prevalent, posing serious risks to public health. Many of these substances, often sold illegally or in convenience stores, are designed to mimic the effects of more familiar drugs, such as opioids, stimulants, and benzodiazepines.
Since 2013, more than 1,000 new and emerging drugs have been identified worldwide, making it crucial for concerned loved ones to stay informed. These drugs, often referred to as designer drugs or new psychoactive substances, are highly dangerous due to their unknown chemical composition and effects.1
Here’s a look at five of the most concerning emerging drugs, how they are abused, and the dangers they present.
1. Nitazenes (“Iso”)
Nitazenes are a class of synthetic opioids that reemerged in 2019 as a replacement for fentanyl. These drugs, which include isotonitazene and metonitazene, are often mixed with or sold as heroin, fentanyl, or counterfeit painkillers. Nitazenes are sometimes marketed as being stronger than fentanyl, a drug already responsible for numerous overdoses.1
Nitazenes are typically abused through injection, snorting, or ingestion. Users may intentionally take nitazenes for their opioid-like effects, but more often, they unknowingly consume them when these drugs are mixed with other opioids like heroin or fentanyl.
Nitazenes are highly potent and can cause respiratory depression, dangerously slow heart rates, and low blood pressure. Their strength makes them extremely dangerous, especially since many users are unaware they are taking them. Overdoses are common and can be fatal.1
2. Tianeptine (“Zaza” or “Tianaa”)
Tianeptine, an antidepressant used in some countries, is not approved in the U.S., but is gaining popularity as a supplement marketed under names like “Zaza” and “Tianaa.” While it is sold as a cognitive enhancer or nootropic, at high doses, tianeptine has opioid-like effects, making it attractive to individuals seeking a legal alternative to opioids.2
Tianeptine is typically abused by taking it in large doses, either in pill or powder form. People use tianeptine to achieve feelings of euphoria, sedation, and pain relief, similar to traditional opioids.2
When taken in high doses, tianeptine can cause both cardiovascular effects and liver and kidney damage. It is highly addictive, and users can develop a dependence on the drug, experiencing withdrawal symptoms similar to those of opioids. These symptoms can include severe cravings, nausea, and anxiety. Tianeptine’s wide availability and its opioid-like effects make it a serious risk, particularly for those seeking to self-medicate.2

3. Synthetic Cannabinoids (“K2” or “Spice”)
Synthetic cannabinoids, known as “K2” or “Spice,” are chemically engineered to copy THC, the active main ingredient in marijuana. However, these substances are far more potent and unpredictable. Often cheaper, synthetic cannabinoids are popular among those trying to avoid detection in drug tests.3
Synthetic cannabinoids are usually smoked or vaped, often as herbal blends or liquids. They are commonly sold in colorful packaging in gas stations and convenience stores, misleading users into thinking they are safe.
These drugs contain compounds that bind to cannabinoid receptors with much greater intensity, leading to more severe adverse effects. Users can experience extreme agitation, paranoia, anxiety, and hallucinations, along with physical issues like rapid heart rate, high blood pressure, chest pain, muscle twitches, and even acute kidney failure.4
4. Synthetic Cathinones (“Bath Salts”)
Synthetic cathinones, commonly referred to as “bath salts,” are powerful stimulants chemically related to the active compounds in the khat plant. These substances have gained popularity as a cheaper alternative to other stimulants, such as cocaine or methamphetamine.
Synthetic cathinones are typically ingested, snorted, or injected. Users seek intense stimulation and euphoria, similar to that of other stimulants. However, many people unknowingly consume synthetic cathinones when they are mixed with drugs like MDMA or cocaine, increasing the risk of overdose.5
Bath salts can cause severe agitation, paranoia, hallucinations, and violent behavior, often leading to dangerous situations where users harm themselves or others. Physical effects include rapid heart rate, elevated blood pressure, and seizures.5
Long-term use can lead to lasting psychological damage and permanent changes to brain chemistry. These substances are also highly addictive, making it difficult for users to stop without professional help. Overdoses are common and often require immediate medical intervention.5
5. Synthetic Benzodiazepines
Synthetic benzodiazepines are chemically altered versions of prescription medications like Xanax and Valium. These drugs are produced illegally and sold as counterfeit pills, often online or by street dealers. They are commonly mixed with opioids or sold to individuals seeking anti-anxiety medication without a prescription.6
Synthetic benzodiazepines are typically consumed either in pill form or injected. People use these drugs for their calming, sedative effects, but because they are often sold as counterfeit versions of prescription medications, users are often unaware of their true strength.6
Synthetic benzodiazepines are highly dangerous due to their unpredictability. When taken in high doses or mixed with other depressants, they can cause over-sedation, coma, or death. The drugs are also highly addictive, leading to physical dependence and dangerous withdrawal symptoms, such as seizures and hallucinations.6
The widespread availability of counterfeit pills containing synthetic benzodiazepines has contributed to an increase in overdose deaths, making them a significant danger in today’s drug market.
Help Your Loved One Get Addiction Treatment at Lumina Recovery
Staying informed about emerging drug trends is essential for protecting your loved ones. New street drugs like nitazenes, tianeptine, and synthetic cannabinoids are becoming increasingly common and pose significant health risks. By understanding these new drug trends, you can better support and protect your loved ones from their potentially life-threatening consequences.
If you suspect your loved one is using any of these emerging drugs, it’s crucial to seek professional help immediately. Lumina Recovery offers specialized drug addiction programs tailored to help individuals recover from opioids, prescription drugs, and other substance abuse challenges.
Contact Lumina Recovery to get the support you need to navigate these challenging times and help your loved one overcome addiction.
Sources:

Your Guide to Mephedrone Addiction
Mephedrone is a synthetic stimulant that has gained notoriety for its potent effects and high potential for abuse. Common mephedrone street names include “Meow Meow” and “M-CAT.”1
As a powerful psychoactive substance, mephedrone produces feelings of euphoria, increased energy, and enhanced sociability, which have made it popular in certain recreational settings, particularly among young adults and within party scenes.
However, this drug’s appeal is accompanied by significant risks, including addiction and severe health consequences. In this guide, we will explore mephedrone’s properties, the reasons it is abused, the signs of addiction, and the challenges of withdrawal, aiming to provide a comprehensive understanding of the dangers associated with this substance.
What Is Mephedrone?
Mephedrone is a synthetic stimulant that belongs to the family of drugs known as cathinones, which are chemically similar to the natural stimulant found in the khat plant. It emerged in the early 2000s as a recreational drug, gaining popularity for its intense and immediate effects. Mephedrone typically comes in the form of a white powder, which can be ingested, snorted, or injected.1
Although mephedrone is widely used in certain social circles, it is illegal in many countries, including the United States, where it is classified as a Schedule I controlled substance, meaning it has no recognized medical use and carries a high potential for abuse.1
Comparing Mephedrone to Other Stimulants
Mephedrone, like stimulants such as MDMA, cocaine, and methamphetamine, increases dopamine, serotonin, and norepinephrine levels in the brain, leading to heightened energy and euphoria.
However, mephedrone is considered more unpredictable and dangerous due to its recent emergence and limited research on its long-term effects. While it shares some effects with MDMA’s empathogenic qualities and cocaine’s intense high, mephedrone’s combination of these traits makes it highly addictive and risky.
Its potential for severe physical and mental health consequences, similar to methamphetamine, underscores the dangers of its use.
Mephedrone Addiction Potential
Mephedrone is known for its powerful stimulant effects, which result from its ability to increase the levels of dopamine, serotonin, and norepinephrine in the brain. These neurotransmitters are associated with feelings of pleasure, reward, and arousal, making mephedrone highly addictive.1
Mephedrone effects on the brain, such as euphoria, heightened energy, and enhanced sociability, are particularly appealing in social and party environments. This makes it an attractive choice for mephedrone chemsex and general misuse.
However, the short-lived mephedrone effects often lead users to take repeated doses in a short period, increasing the risk of developing a dependence. The intense cravings and psychological dependence that can result from mephedrone use make it a particularly dangerous substance, with a high potential for addiction and long-term health consequences.
Signs of Mephedrone Addiction
Recognizing the signs of mephedrone addiction is crucial for early intervention and treatment. Below are key indicators that someone may be struggling with an addiction to this powerful stimulant:
- Compulsive Drug-Seeking Behavior
Individuals may go to great lengths to obtain and use mephedrone, often neglecting responsibilities and personal relationships. - Social Withdrawal
Addicted users might withdraw from social interactions that do not involve drug use, isolating themselves from friends and family. - Physical Deterioration
Noticeable signs include rapid weight loss, poor hygiene, and chronic insomnia, reflecting the physical toll of addiction. - Psychological Symptoms
Intense cravings, anxiety, depression, and paranoia are common, often worsening as the addiction deepens. - Engagement in Risky Behaviors
Users may take the drug in dangerous situations or mix it with other substances, increasing the risk of severe consequences.

Side Effects of Mephedrone Use
Mephedrone use can lead to a variety of serious health issues, both in the short and long term. The following are some of the most common and concerning side effects associated with the drug:2
- Increased Heart Rate and Blood Pressure: Immediate mephedrone effects that can lead to cardiovascular strain
- Hyperactivity and Euphoria: Often accompanied by agitation, making users prone to impulsive actions
- Anxiety and Agitation: Short-term use can heighten feelings of anxiety and restlessness
- Long-Term Cardiovascular Problems: Prolonged use can damage the heart and blood vessels
- Kidney Damage: Chronic use may lead to significant renal issues
- Cognitive Impairments: Long-term abuse can result in memory problems and difficulty concentrating
- Mental Health Issues: Persistent use is associated with depression, anxiety disorders, and in some cases, psychosis
- Engagement in Risky Behaviors: Mixing substances like mephedrone and alcohol can amplify the harmful effects of both substances
Withdrawal From Mephedrone
Withdrawal from mephedrone can be a challenging and distressing process, characterized by a range of physical and psychological symptoms.
As the body and brain adjust to the absence of the drug, individuals may experience intense cravings, fatigue, depression, anxiety, and irritability. These symptoms often emerge within hours to days after the last use and can persist for several weeks, depending on the severity of the addiction. Many users report feeling irritable, restless, and unable to concentrate, which can make it difficult to function in daily life.3
Additionally, the psychological aspect of withdrawal can be particularly tough, with some individuals experiencing vivid nightmares and feelings of paranoia.
Given the intensity of these symptoms, it is often recommended that individuals seek medical supervision to manage withdrawal safely and effectively, reducing the risk of relapse and helping to address the underlying issues that contributed to the addiction.
Find Hope and Healing at Lumina Recovery
If you or someone you love is struggling with mephedrone addiction, it’s essential to seek professional help to ensure a safe and successful recovery.
Lumina Recovery’s medically supervised detox programs are designed to help you manage withdrawal symptoms safely and effectively, with round-the-clock care from experienced medical professionals. We offer comprehensive inpatient addiction treatment programs that provide the support and structure needed to overcome addiction.
We understand the challenges of addiction and are committed to helping you regain control of your life. Reach out to us today and let us guide you on your journey to healing.
Sources:

Dexedrine Abuse: Side Effects, Withdrawal, & Treatment
Dexedrine, a brand name for dextroamphetamine, is a prescription stimulant widely used to treat conditions like attention-deficit/hyperactivity disorder (ADHD) and narcolepsy. By increasing the levels of certain chemicals in the brain, Dexedrine helps improve focus, attention, and impulse control.
However, while this medication can be highly effective when used as prescribed, it also carries a significant risk of abuse due to its potent stimulating effects. For some, the desire to enhance focus, energy, or mood can lead to the misuse of Dexedrine, resulting in serious consequences.
What Is Dexedrine?
Dexedrine is a stimulant medication that affects the central nervous system. Typically, it is prescribed to individuals with ADHD or narcolepsy, helping them manage symptoms by improving concentration and reducing impulsivity. When used as directed by a healthcare provider, Dexedrine can be a valuable tool in managing these conditions.
However, problems arise when Dexedrine is used in ways that deviate from its prescribed purpose. Abuse occurs when individuals take higher doses than recommended, use the drug without a prescription, or consume it for non-medical reasons, such as staying awake longer or enhancing academic or professional performance. This misuse is dangerous, as it significantly increases the risk of developing serious health issues, including dependency and addiction.
Dexedrine Side Effects
Like many prescription medications, Dexedrine can cause side effects. It’s important to be aware of these potential reactions and consult with your doctor if you experience any of the following:1
- Dry mouth
- Nausea
- Dizziness
- Trouble sleeping
- Weight loss
- Increased heart rate
- Restlessness
- Anxiety
- Mood changes
- Headache
- Shortness of breath
- Chest pain
- Uncontrollable shaking
- Seizures
If any side effects become severe or concerning, seek medical advice immediately.
Additionally, the misuse or abuse of amphetamines can lead to severe, potentially life-threatening heart and blood pressure issues.2
Is Dexedrine Addictive?
Yes, Dexedrine is addictive, especially when it is abused. The drug’s ability to increase dopamine levels in the brain creates a sense of euphoria, which can lead to repeated use and, eventually, Dexedrine addiction.
Over time, the brain becomes reliant on Dexedrine to experience these heightened levels of focus and energy, leading to physical and psychological dependence.
Once dependency sets in, stopping or reducing Dexedrine use can result in withdrawal symptoms, making it challenging for individuals to quit without professional help. This addictive potential makes it crucial to use Dexedrine strictly as prescribed and to be aware of the risks associated with its misuse.
Dexedrine Withdrawal
When someone who has been taking an amphetamine like Dexedrine reduces their dosage or stops taking the drug altogether, their body and brain must adjust to the absence of the stimulant. This adjustment period is known as withdrawal.
Unlike those who use Dexedrine as prescribed, individuals who abuse the drug often experience more intense and challenging withdrawal symptoms.
The body, having become accustomed to the artificial stimulation provided by Dexedrine, reacts strongly when the drug is no longer present, leading to a range of physical and psychological symptoms, including:2
- Severe tiredness
- Sleep disturbances such as irregular sleep patterns or insomnia
- Mental health issues such as depression

Dexedrine Addiction Treatment
Effective treatment for Dexedrine addiction involves a comprehensive approach, combining medically supervised detox, behavioral therapy, and ongoing support. For many individuals, inpatient treatment provides the structured environment necessary for successful recovery.
Medically supervised detox is the first critical step, helping to safely manage withdrawal symptoms and minimize the risk of complications. Once detox is complete, individuals can move on to the next phase of care.
In inpatient treatment, individuals benefit from 24/7 medical supervision, structured daily routines, and intensive therapeutic interventions. This setting provides a safe space away from outside stressors and temptations, allowing patients to focus fully on recovery. Behavioral therapies, such as cognitive behavioral therapy (CBT) and group counseling, are integral to inpatient care, helping individuals develop coping strategies, address underlying issues, and build a foundation for long-term recovery.
After completing inpatient treatment, ongoing support through outpatient programs or aftercare services is crucial. These programs offer continued therapy and resources to help individuals stay on track, reduce the risk of relapse, and maintain long-term sobriety.
Take the First Step Toward Recovery From Dexedrine Abuse
Dexedrine abuse can lead to severe physical and psychological consequences, including Dexedrine addiction, health issues, and challenging withdrawal symptoms. If you or someone you know is struggling with Dexedrine abuse, it’s essential to seek professional help.
At Lumina Recovery, we offer comprehensive treatment options, including medically supervised detox to safely manage withdrawal and tailored inpatient and outpatient rehabilitation programs to support long-term recovery.
Our dedicated team is here to guide you every step of the way, providing the care and support needed to achieve a healthier, drug-free life.
Don’t hesitate to reach out to Lumina Recovery today to start your journey to recovery.
Sources:

Recognizing Fentanyl Fold and Subtle Signs of Fentanyl Use
Addiction to fentanyl, a powerful synthetic opioid, has been on the rise, leading to devastating effects on individuals and their loved ones. Among the many signs of fentanyl abuse, one alarming and increasingly recognized phenomenon is known as the “fentanyl fold” or “the fentanyl bend over.”
It is crucial to understand what the fentanyl fold is, what causes it, how to recognize other, less obvious signs of fentanyl abuse, and how to approach a loved one about getting help for their addiction.
What Is Fentanyl Fold?
The “fentanyl fold,” also referred to as “the fentanyl bend over,” is a phenomenon where individuals under the influence of fentanyl appear to be hunched or slumped over in a folded position. This posture, while unnatural, can last for extended periods as the person struggles to regain control of their body.1
This physical stance is often seen in public spaces, adding to the growing visibility of the opioid crisis. The fentanyl fold doesn’t just signal intoxication, it reflects the overwhelming impact that fentanyl has on the body’s motor functions.
The fentanyl fold can be an early sign that someone is on the edge of a drug overdose or respiratory failure, which is why this posture should never be ignored. It’s essential for people around those exhibiting this behavior to recognize the severity of the situation and, if necessary, contact emergency services.
What Causes the Fentanyl Fold?
The fentanyl fold is primarily caused by fentanyl’s overwhelming sedative properties. As a synthetic opioid, fentanyl is 50 times more potent than morphine, which means its effects on the body are stronger and quicker.2
When fentanyl enters the bloodstream, it quickly crosses into the brain, where it binds to opioid receptors. These receptors are involved in regulating not only pain but also essential bodily functions like breathing, heart rate, and muscle coordination.2
One of fentanyl’s most pronounced effects is respiratory depression, where breathing slows to a dangerously low rate. This lack of oxygen to the brain and muscles can contribute to the slackening of muscle tone, making it difficult for individuals to maintain their posture. While other opioids can cause similar effects, fentanyl is so potent that the body’s muscle control deteriorates rapidly, leading to the telltale “folded” posture.2
In addition to respiratory depression, fentanyl causes extreme sedation. The euphoric high that comes from using the drug is paired with a feeling of profound drowsiness. In many cases, users are unable to stay awake or alert, even while sitting or standing. This intense sedation leads to the slumped-over, folded posture that fentanyl users often display.2
4 Less Obvious Signs of Fentanyl Abuse
While some signs of fentanyl abuse, such as the fentanyl fold, are more visible, many indicators are subtle and harder to detect. Recognizing these less obvious signs can be critical in identifying fentanyl addiction early and helping someone seek the necessary support:2
1. Changes in Behavior and Routine
One of the early warning signs of fentanyl abuse is a noticeable shift in behavior or daily routine. People struggling with substance use disorder may begin neglecting their responsibilities at work, school, or home. You might notice increased absenteeism or lateness, a decline in performance, or a lack of interest in activities they once enjoyed. These changes can happen gradually, making it easy to dismiss them as stress or fatigue, but they are often linked to the compulsive nature of drug seeking and use.
2. Physical Symptoms of Use and Withdrawal
Fentanyl abuse can cause various physical symptoms, some of which may not be immediately linked to drug use. These symptoms include drowsiness, nausea, constipation, and confusion. Over time, the body becomes reliant on the drug, and withdrawal symptoms can start to appear if fentanyl is not used, such as chills, sweating, or restlessness.
3. Emotional Instability
Fentanyl use can lead to emotional ups and downs that seem unpredictable. Someone may experience extreme happiness or euphoria shortly after using the drug, followed by sedation or depressive episodes as the drug’s effects wear off. These mood swings can disrupt relationships, create tension, and lead to isolation as the person becomes more focused on obtaining and using fentanyl.
4. Increased Secrecy and Isolation
As fentanyl addiction takes hold, individuals may become more secretive and isolated. This behavior often stems from shame, fear of being judged, or an attempt to hide their drug use. You may notice them avoiding social gatherings, withdrawing from family events, or spending long periods alone. They may also lie about their whereabouts or activities.

Talking to a Loved One About Getting Help
Addressing fentanyl addiction is never easy, especially when someone you care about is caught in its grip. However, it’s crucial to have a conversation with your loved one about seeking help for their addiction. Here are some tips for approaching this delicate situation:
- Pick the right moment. Avoid confronting someone when they’re under the influence of fentanyl or in a highly emotional state. Instead, choose a time when they are relatively calm and sober.
- Express concern without judgment. When discussing addiction, it’s vital to avoid coming across as accusatory or judgmental. Instead, express your concern out of love and worry for their well-being. Use “I” statements, such as “I’m worried about you,” rather than “You’re ruining your life.”
- Educate yourself. Before starting the conversation, learn as much as you can about fentanyl addiction, its effects, and treatment options. Being informed shows that you’re serious about helping and gives you the knowledge to answer any questions they may have.
- Have resources ready. If your loved one is open to the idea of seeking help, be prepared with information on treatment centers, group therapy, or detox programs. Having these resources ready can ease their transition into accepting help.
- Be patient. Addiction is a complex disease, and recovery doesn’t happen overnight. Even if your loved one is not ready to seek help right away, the conversation you have started can plant the seed for future change. Continue to express your support and remind them that help is available when they are ready.
Ready to Get Help for Fentanyl Addiction? Lumina Recovery Is Here
Fentanyl addiction is a serious and life-threatening condition, and signs like the fentanyl fold can indicate that someone is in deep need of help. Beyond these more obvious signs, there are many other subtle indicators of fentanyl use, and recognizing them is critical in addressing the addiction early.
Through holistic opioid addiction treatment, Lumina Recovery is ready to help you or a loved one at any step of the healing process from medically assisted detox to aftercare, and everything in between.
Reach out today to support your loved one in taking the critical steps toward recovery and reclaiming their health and future.
Sources:

The Benefits of Group Therapy for Addiction Recovery
The power of group therapy for addiction recovery can be transformative. There’s a saying often heard in addiction circles: “We’re only as sick as our secrets.” In the safe and supportive environment of addiction therapy groups, individuals can share their struggles and vulnerabilities without fear of judgment. By bringing hidden thoughts and feelings into the open, people can begin to heal, finding strength and comfort in the shared experiences of others.
It’s natural to feel some confusion or hesitation about how group therapy can aid in addiction recovery. Many individuals struggling with substance abuse fear the isolation that addiction brings and the vulnerability required to share their deepest, darkest secrets in a group setting. You might wonder, “Can I really be that honest with so many new people? How can sharing in a group possibly help my recovery?”
The first step is finding the right group therapist or facilitator. It’s essential to choose someone who understands how to effectively use group dynamics for healing and approaches the process with empathy and compassion. A good facilitator balances authority with a gentle and respectful tone, creating a safe space for everyone to share openly.
Once you find a group that aligns with your treatment goals, remember that your experience and healing are within your control. Being open and sharing a part of yourself is crucial. If you hold back, it may be difficult for the group to provide the support you need. The key to benefiting from addiction group therapy lies in your willingness to show up, be seen, and participate. Your path to recovery starts with taking that brave step to share—often, the answer is in your own hands.
What Is Group Therapy?
Group therapy is a specialized counseling approach designed to help individuals address psychological challenges, such as substance abuse and other mental health issues. Sessions typically involve 6–12 participants, along with one or two therapists trained in group dynamics.
These therapists provide professional support by guiding discussions, ensuring every voice is heard, and encouraging members to draw strength, build connections, and gain insights from each other’s experiences. This collaborative environment helps break the isolation often caused by addiction, creating a sense of belonging and mutual support.
When you first join a group, the therapist will invite you to introduce yourself and share some of your thoughts or experiences. This helps establish an open and welcoming atmosphere, allowing you to begin building trust with others. By sharing and listening, you contribute to a supportive community where everyone feels understood and valued.
What Are the Benefits of Group Therapy?
Some may worry that group therapy for drug addiction or alcohol addiction won’t be as effective as individual therapy due to less one-on-one time with a therapist. However, group therapy can be just as impactful, if not more so, because it mirrors the social world we live in. Group therapy reflects real-life interactions and teaches us valuable lessons, which we’ll cover below.
You Are Not Alone
This realization is crucial for individuals struggling with substance abuse, who often feel deep shame and guilt. These emotions may originate from past trauma or abuse that they’ve never felt safe enough to share, leading them to believe, “I’m the only one going through this.” In group therapy, connecting with others facing similar challenges can offer immense comfort and a powerful sense of belonging.
You’ll Solve Problems Together
When individuals share their struggles and work collaboratively to find solutions, they create a bond of trust. This shared experience breaks down feelings of isolation and builds a supportive community where members learn from each other and share ways to cope with the ups and downs of life. Being connected to others, who genuinely understand your challenges, can provide the encouragement and motivation needed to stay committed to your recovery journey.
You’ll Improve Your Communication Skills
Reflecting on and sharing your journey and successes invites valuable feedback and advice. If someone misunderstands you, it provides an opportunity to refine your communication skills and how you interact with others. In a group setting, you also learn to practice active listening and empathy, which enhances your ability to respond thoughtfully and with emotional openness, encouraging more authentic relationships.

How to Get the Most Out of Group Therapy
You deserve to be seen and heard. Here are some ways to help you get the most benefit from attending group therapy for alcohol addiction or drug addiction.
Be Open and Honest
Being around others who share your feelings can inspire bravery and honesty. Even sharing just one sentence about how you feel can encourage more reserved members to open up. The more you share honestly, the more support you’ll receive from the group. As you express yourself, you’ll begin to heal, and start to gain insights into your experiences, marking the start of your journey to rediscovering yourself.
Respect the Privacy of Fellow Members
Confidentiality is crucial for creating a safe and trusting environment where everyone feels secure sharing their experiences. It takes courage to open up about sensitive, private matters, so it’s important to be respectful and considerate of both yourself and others.
Listen to and Support Others
Simply being present and genuinely listening to someone with similar struggles can make them feel seen and valued. Your attentive listening and support can offer fellow members the confidence and encouragement they need to remain committed to their challenging journey toward wholeness.
Be Patient With the Process
Sharing your thoughts and feelings with strangers may feel awkward at first, but over time it will likely become easier and more meaningful. Embrace the process with kindness towards yourself and others. Each session is a step toward understanding and healing. Trust that, with time, you will grow stronger, more resilient, and closer to your goals.
Group Therapy at Lumina Recovery: Discover Your True Voice
At Lumina Recovery, our group therapy sessions are thoughtfully designed to forge deep connections among participants. Here, stories are shared, challenges are understood, and victories are celebrated together. Our dedicated therapists create a nurturing environment where honesty, empathy, and understanding are at the heart of every session. In our addiction therapy groups, you’re not just engaging in therapy—you’re becoming part of a supportive family that grows together, guiding you toward a brighter, addiction-free future.
Reach out to our team today. We are here to support you on your healing journey and help you achieve true transformation.

Is Buprenorphine Addictive? Risks and Benefits
When facing opioid addiction, finding an effective treatment can be a critical step toward recovery. One of the most widely used medications in opioid treatment programs is buprenorphine.
This drug has provided countless individuals with a way to manage withdrawal symptoms, reduce cravings, and regain control of their lives. Understanding what buprenorphine is, how it is used, its potential for misuse, and the importance of medical guidance is essential.
What Is Buprenorphine?
Buprenorphine is a prescription medication primarily used in treating addiction to opioids. It’s a partial opioid agonist that attaches to the brain receptors as other opioids but with less intensity. This makes it very effective in reducing cravings and withdrawal symptoms without producing a similar “high” as drugs like heroin or prescription painkillers.1
Because of its unique properties, those struggling with opioid addiction can benefit from using buprenorphine as a key component of medication-assisted treatment (MAT). MAT combines medication with counseling and behavioral therapies to offer a comprehensive approach to recovery. Buprenorphine is often prescribed in combination with naloxone, another drug that blocks the effects of opioids, to further prevent misuse.1
What Is Buprenorphine Used For?
The main goal of buprenorphine is to assist individuals in controlling opioid dependence. It connects to opioid receptors without fully triggering them, helping lessen the strong urges that may result in relapse. This allows individuals to focus on their recovery journey, attend therapy sessions, and rebuild their lives.
However, buprenorphine for pain management is common as well. Its pain-relieving properties make it a viable option for individuals who need pain relief but may be at risk of opioid misuse. When prescribed for pain, the dosage and administration are carefully managed to minimize the risk of addiction.2
Potential for Misuse
Buprenorphine is a valuable tool in treating opioid addiction, but it carries the potential for misuse if not used as directed. While the drug’s “ceiling effect” makes it safer than other opioids, individuals can still misuse it by taking larger doses or combining it with other substances. For some, buprenorphine’s ability to bind to opioid receptors may provide mild euphoria, leading to misuse, especially by those not prescribed the drug.3
Misuse often occurs when buprenorphine is taken in non-prescribed amounts or obtained illegally. Additionally, combining buprenorphine with alcohol or benzodiazepines can increase the risk of respiratory issues and overdose.
It’s crucial to follow a doctor’s guidance to minimize risks, as misuse can lead to physical dependence and withdrawal symptoms. Under medical supervision, however, buprenorphine is highly effective in controlling opioid cravings and withdrawal, making it a key part of a comprehensive treatment plan.

Buprenorphine Addiction
Buprenorphine’s partial agonist properties make it less likely to cause addiction compared to full opioids, but the risk still exists. Physical dependence can develop if the drug is taken inappropriately or for extended periods. Although buprenorphine produces less euphoria than opioids like heroin, it can still lead to dependence when misused, particularly if someone takes more than prescribed or uses the drug without supervision.3
Over time, tolerance to buprenorphine can develop, meaning that a person may need higher doses to achieve the same effect. This can increase the risk of dependence and withdrawal symptoms. Additionally, psychological dependence can also occur, where individuals begin to rely on buprenorphine as a way to cope with emotional stress or discomfort, rather than addressing underlying issues.
In a clinical setting, the chances of addiction are low because doctors monitor and adjust dosages carefully. When used correctly, buprenorphine is an effective tool in managing opioid addiction. If you or a loved one is concerned about buprenorphine use, seeking medical help is the best way to ensure it’s used safely in recovery.3
Buprenorphine Withdrawal
If someone abruptly stops taking buprenorphine after long-term use, they may experience withdrawal symptoms. These can include nausea, sweating, muscle aches, and insomnia. While buprenorphine withdrawal is generally milder than withdrawal from full opioids, it can still be uncomfortable and challenging.3
The intensity and duration of withdrawal symptoms can vary depending on factors like the length of time the individual was taking buprenorphine and the dosage they were on.
It’s essential to consult with a medical professional if you or someone you know is considering stopping buprenorphine use. Tapering off the drug under the guidance of a healthcare provider can help minimize withdrawal symptoms and ensure a safe transition.
The Importance of Medical Guidance
Buprenorphine can have a great impact on opioid addiction, but like all medications, it must be used responsibly. When prescribed and taken under the supervision of a healthcare provider, buprenorphine can help individuals regain control of their lives and break free from the cycle of opioid addiction.
It’s critical to avoid self-medicating or using buprenorphine outside of a structured treatment program. Misusing the drug can lead to buprenorphine side effects, dependency, and withdrawal, making the recovery process even more challenging.
If you are concerned about your buprenorphine use or believe it has become difficult to manage, reaching out to a specialist at Lumina Recovery is a great step toward finding support.
Understand Your Options for Buprenorphine Addiction With Lumina Recovery
While buprenorphine is highly effective for treating opioid addiction, it must be taken under medical supervision to reduce the risk of misuse or dependence. If you’re wondering, “is buprenorphine addictive?”, the answer is that it can be, but with proper care and oversight, the benefits often far outweigh the risks.
At Lumina Recovery, we believe that recovery is possible, and we’re here to guide you every step of the way from initial detox to medication-assisted treatment (MAT) for opioid addiction.
If you or someone you love is struggling with buprenorphine use or opioid addiction, reach out to our specialists today for compassionate, evidence-based care.
Sources:

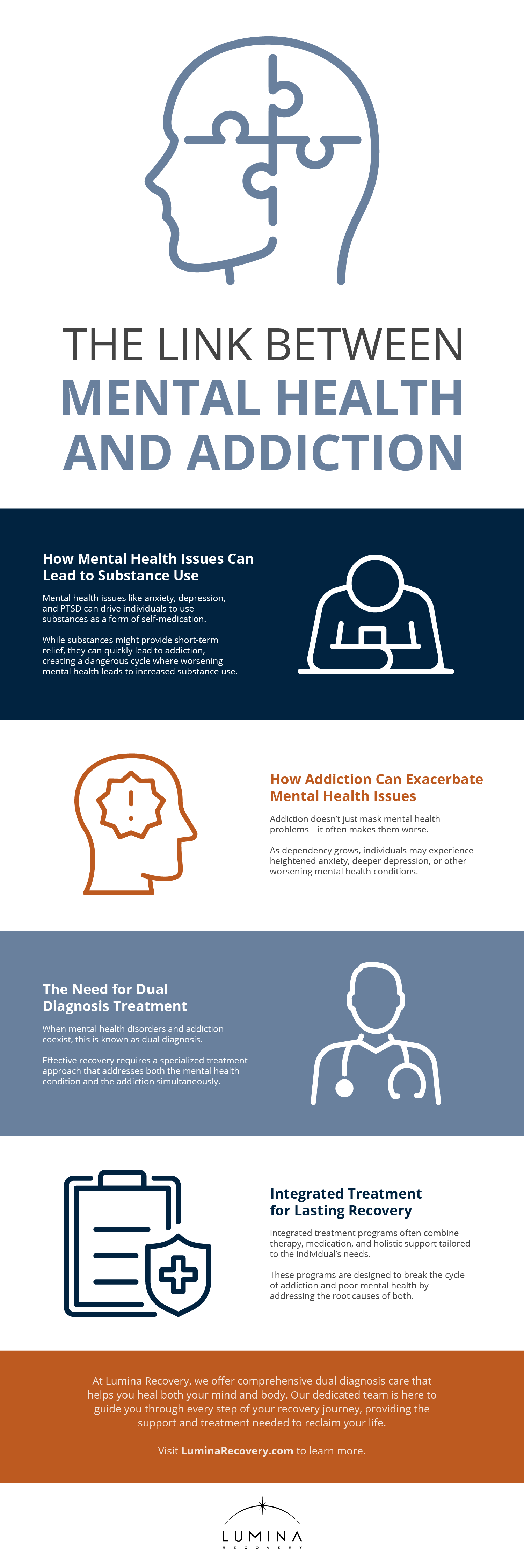
The Link Between Mental Health and Addiction
Mental health and addiction are intricately linked, creating a complex relationship that can be challenging to navigate. Understanding how these two aspects of health interact is crucial for anyone seeking to break free from the cycle and achieve lasting recovery.
Mental Health and Self-Medication
When struggling with mental health issues like anxiety, depression, or PTSD, people often seek relief in substances such as drugs or alcohol. This is known as self-medication. While it may provide temporary comfort, it doesn’t address the underlying mental health problems and can lead to addiction.
How Addiction Develops
Self-medicating with substances can quickly turn into a dependency. Over time, the body and mind begin to rely on these substances just to feel normal, leading to a drug or alcohol addiction.
The Dangerous Feedback Loop
Addiction can not only stem from poor mental health—it can also make it worse. As addiction progresses, it can exacerbate mental health issues, creating a cycle where worsening mental health leads to increased substance use, and vice versa. This loop is challenging to break without professional help.
Understanding Dual Diagnosis
When someone is dealing with both a mental health disorder and a substance use disorder, this is known as a dual diagnosis. Dual diagnosis requires specialized, integrated treatment that addresses both issues simultaneously to ensure effective recovery.
Breaking the Cycle
Effective recovery is possible with the right approach. Integrated treatment programs that address both mental health and addiction are essential. These dual diagnosis treatment programs combine therapy, support, and sometimes medication to help individuals break free from the cycle and regain control of their lives.
Dual Diagnosis Care at Lumina Recovery
At Lumina Recovery, we understand the complexities of dual diagnosis and are here to support you every step of the way. Our dual diagnosis treatment programs are designed to address both your addiction and mental health simultaneously, giving you the best chance for a lasting recovery. Don’t let the cycle continue—reach out to Lumina Recovery today and start your journey toward a healthier, more balanced life.
Additional Resources
Once you have completed your rehabilitation program at one of our drug and alcohol treatment centers, you should try to surround yourself with people who can encourage you to stay sober. Many people find that support groups are the best source of encouragement. You can find hundreds of support groups and meetings in your community. Our drug addiction treatment centers stress the importance of personal chemical dependency resources, especially when you are new to sobriety. Below are various addiction and mental health resources for people in recovery who want additional support.
Christian Addiction Recovery Resources
Our substance abuse services aren’t limited to specific programs, but rather we believe in the importance of incorporating faith-based programs to promote spiritual healing, like our Faith in Recovery program.
With that said, below are some faith-based addiction recovery resources that could help you in your spiritual healing from addiction:
- Battlefield of the Mind by Joyce Meyer
- Boundaries by Dr. Henry Cloud & Dr. John Townsend
- Christian Families in Recovery: A Guide for Addiction, Recovery, and Intervention Using God’s Tools of Redemption by Robert and Stephanie Tucker
- Club New Life Christian Ministry for Addiction and Recovery
- Lost & Found: Recovery in Christ by Bruce Stanley
- Overcoming Emotional Obstacles through Faith: Navigating the Mind Field by Anthony Acampora, Director of Banyan’s Faith in Recovery Program
- The Case for Christ by Lee Strobel
Mental Health Resources for Recovery
Lumina Recovery consist of both mental health and substance abuse treatment facilities, meaning we offer mental health resources as well as chemical dependency resources. What’s more, addiction often co-occurs with mental illness, making these resources ever more important.
Below are some resources for mental health recovery that can help you or your loved one:
- This Emotional Life video series
- No Kidding, Me 2!! with Joe Pantoliano
- Dare: The New Way to End Anxiety and Stop Panic Attacks by Barry McDonagh
- Pleasure Unwoven: An Explanation of the Brain Disease of Addiction by Kevin McCauley
- Declutter Your Mind: How to Stop Worrying, Relieve Anxiety, and Eliminate Negative Thinking by S.J. Scott and Barrie Davenport
Call Us Today – (877) 716-7515

