
Our Addiction Resources
Navigating the world of addiction and recovery can be overwhelming. We’re here to provide clear, compassionate education and guidance. From practical advice for maintaining sobriety to informational guidance on the long-term effects of substance abuse, our content is a beacon of hope and understanding.
Our Team is Ready are ready to take your call
Call us Today!
or we can call you. Fill out form below
Our Blog

Signs and Symptoms of Crack Addiction
Crack cocaine, often just called crack, is a highly addictive and powerful drug variant of cocaine. The substance gets its name from the crackling sound it makes when smoked. The effects of crack cocaine are known for delivering intense but short-lived, euphoric highs, making it particularly susceptible to repeated use and substance abuse.
This combined with severe withdrawal symptoms makes crack cocaine addiction one of the most challenging addictions to confront, but not impossible with the right addiction treatment from medical professionals.
Our goal is to provide valuable knowledge on the signs and symptoms of crack addiction for those who suspect that someone close to them might be struggling or are concerned about their own use.
9 Signs of Crack Cocaine Addiction
Crack abuse, like other substance use disorders, can be identified by a variety of symptoms. Recognizing these symptoms of crack use, whether in yourself or a loved one, is crucial for addressing the issue and seeking help. Those addicted to crack may show signs that include:1
- Tolerance for the drug. Over time, individuals may require larger amounts of cocaine to achieve the same high. This increased tolerance indicates that the body is adapting to the drug, necessitating higher doses for the desired effect.
- Inability to stop or reduce usage. An individual struggling with cocaine addiction often finds it difficult to stop or cut back their usage, even if they want to. The compulsion to use the drug can override their desire to quit.
- Experiencing withdrawal symptoms. When cocaine usage stops, withdrawal symptoms can appear, including fatigue, depression, and increased appetite. These symptoms often drive individuals back to using the drug to avoid discomfort.
- Desire to use despite health issues. Cocaine can cause numerous health problems, such as cardiovascular issues and mental health disorders. Despite recognizing these problems, individuals with an addiction may continue using cocaine, prioritizing the drug over their health.
- Negative impact on life. Cocaine addiction can negatively affect one’s quality of life, relationships, and employment. An individual might face conflicts with loved ones, job loss, or a decline in overall well-being due to their drug use.
- Spending excessive time and money on cocaine. Individuals may spend substantial time and money seeking and using cocaine. This can lead to financial problems and neglect of important responsibilities.
- Having psychosis and hallucinations. In severe cases, cocaine addiction can lead to psychosis or hallucinations, where individuals might hear or see things that aren’t there. These episodes can be frightening and dangerous.
- Being irritable or anxious. Cocaine can induce irritability or heightened anxiety, especially during withdrawal or when the drug is wearing off. These mood changes can be sudden and extreme.
- Disappearing for binges. It’s common for individuals with a cocaine addiction to disappear for extended periods, often for binge sessions. This behavior can alarm loved ones and disrupt daily life.
Symptoms of Crack Abuse
Crack cocaine abuse can manifest through a variety of physical and psychological symptoms that can significantly impact an individual’s life. Recognizing these symptoms early is crucial for seeking timely treatments for drug addiction and initiating the path to recovery:2
Psychological Symptoms
- Users often experience paranoia and anxiety attacks, which can be severe and debilitating.
- Both auditory and visual hallucinations are common, further distorting the user’s sense of reality.
- Mood swings can be drastic and unpredictable, leading to aggression and irritability without much provocation.
- The highs from the drug are often followed by periods of intense anxiety and depression once the effects wear off.
- Impaired judgment can cause decision-making skills to be significantly compromised, leading to poor choices and dangerous behaviors.
- Users may exhibit strange or repetitive behaviors, such as constant talking or fixating on particular tasks.

Physical Symptoms
- Significant and unhealthy weight loss is common due to reduced appetite.
- Users often experience an increased heart rate, which can be taxing on the cardiovascular system.
- Gastrointestinal issues including nausea and abdominal pain are frequent, and appetite is generally diminished.
- Neurological impacts including headaches, seizures, and strokes may occur, especially with frequent use.
- Smoking crack cocaine can lead to respiratory problems, including diseases like bronchitis or pneumonia.
- Cardiovascular strain leads to an increased risk of chest pains, heart arrhythmias, and heart attacks.
- Systemic damage from long-term use can lead to severe conditions like hepatitis, gangrene of the bowels, and a weakened immune system due to overall health degradation.
Ways to Get Help for Crack Addiction
Recognizing the need for help is a critical step toward recovery. If you or a loved one is struggling with crack addiction, there are several avenues for support:
Professional Counseling: Addiction specialists can provide therapy that targets the psychological aspects of addiction.
Rehabilitation Programs: These programs offer structured support and are equipped to handle the intense physical withdrawal symptoms and provide psychological counseling.
Support Groups: Groups like Narcotics Anonymous (NA) offer community support and a platform to share experiences, which can be instrumental in the recovery process.
Medical Intervention: In some cases, medical intervention may be necessary to manage withdrawal symptoms safely. Medications can also be prescribed to help reduce cravings and manage mental health issues.
Holistic Therapies: Activities like yoga, meditation, and acupuncture have proven beneficial for some individuals by reducing stress and improving mental health.
Educational Workshops: These can provide both the addict and their loved ones with information about the addiction process and how to cope with its challenges.
Embark on Your Path to Sobriety With Lumina Recovery
Crack addiction is a serious condition that can devastate lives, but understanding the signs and symptoms is the first step toward recovery. Whether you are worried about a loved one or yourself, it is crucial to take action and seek help.
Lumina Recovery tailors our crack and cocaine addiction treatment programs to the individual’s unique needs to find the root cause of addiction. The journey to recovery starts with one brave step forward and we are ready to help you.
If you or someone you know is struggling with addiction, reach out to our professionals for help today.
Sources:

Meth Withdrawal: Symptoms and Recovery Insights
Methamphetamine is a highly addictive stimulant, and when someone decides to confront their substance abuse, the first step towards recovery often involves facing withdrawal.
Experiencing withdrawal symptoms of methamphetamine can be daunting and uncomfortable, but understanding the symptoms and the timeline can help prepare individuals and their loved ones for what lies ahead.
Meth Withdrawal Timeline and Symptoms
Methamphetamine withdrawal symptoms are a significant challenge that affect both the body and mind. The timeline for withdrawal includes an acute phase followed by a subacute phase, each characterized by specific symptoms and levels of intensity:1
Acute Phase: Days 1-10
The acute withdrawal symptoms of methamphetamine addiction are the most intense and begin almost immediately after cessation of use. It generally lasts between 7 to 10 days, characterized by a peak in symptoms that typically occurs around 24 hours after the last dose. Key symptoms during this phase include:
- Increased Appetite: A marked increase in appetite is common as the body adjusts to the absence of meth, which typically suppresses hunger.
- Meth Craving: Cravings are intense during this phase as the body reacts to the absence of the stimulant it has grown accustomed to.
- Depression-Related Symptoms: Individuals may experience severe depressive symptoms, including profound sadness, lack of motivation, and in some cases, suicidal thoughts.
These symptoms, particularly cravings and depressive symptoms, are at their most severe in the first few days and gradually begin to decline as the acute phase progresses.
Subacute Phase: Days 11-21
Following the acute phase, meth withdrawal enters a subacute phase that can last up to 3 weeks. During this period, symptoms become milder and more stable but can persist, presenting challenges in recovery:
- Stable Mood Changes: While the intensity decreases, mood swings such as irritability, depression, and an inability to experience pleasure (anhedonia) can continue.
- Persistent Cravings: Though reduced, cravings for methamphetamine may persist and can still pose a significant risk for relapse.
- Continued Sleep Disturbances: Issues with sleep may continue, including difficulty falling asleep or sleeping excessively.
- Lethargy: A general feeling of tiredness remains, even though less severe than during the acute phase.
Psychopathology and Psychotic Symptoms
Meth withdrawal can also be associated with significant psychopathology and psychotic symptoms. These can include:
- Decreased Psychopathology: Signs of mental health issues tend to decrease substantially after a week or more of abstinence.
- Psychotic Symptoms: A substantial portion of meth-dependent individuals experience psychotic symptoms such as paranoia, hallucinations, and extreme hostility. These symptoms can be exacerbated during withdrawal and require careful management.
Craving and Risk of Relapse
Craving for meth is a critical aspect of withdrawal that extends throughout the acute and subacute phases and beyond. Persistent craving significantly contributes to the high rate of relapse observed among meth users. The period between days 7 and 14 of abstinence is particularly vulnerable, with heightened craving and depressive symptoms making relapse more likely.
Getting Treatment for Meth Addiction
Overcoming methamphetamine addiction is a challenging journey that begins with recognizing the need for help and seeking appropriate addiction treatment. One of the most critical steps in this process is undergoing supervised detoxification.
What Is Supervised Detox?
Supervised detox is a medically managed withdrawal process designed to safely help individuals stop using meth while managing the acute and potentially dangerous physical and psychological effects of withdrawal. This process is conducted in a controlled environment, such as a detox center or hospital, where healthcare professionals monitor and support the patients throughout.
The detox process typically begins with an assessment, where medical professionals evaluate the patient’s health status, meth use history, and any co-occurring mental health conditions. This assessment helps the team create a personalized detox plan that addresses the individual’s specific needs.
Following the assessment, the detox phase starts. This involves the patient staying at the detox facility while their body clears itself of meth. Throughout this period, the patient’s vital signs are monitored regularly, and interventions are made to manage withdrawal symptoms. This phase can last from a few days to several weeks, depending on the severity of the addiction and the individual’s physical health.

4 Benefits of Supervised Detox
- Medical Safety
Withdrawal from meth can be physically and emotionally taxing, and in some cases, dangerous. Supervised detox provides continuous medical supervision to address any complications that arise during the withdrawal process. This includes management of symptoms such as dehydration, extreme fatigue, and psychotic episodes, ensuring the patient’s safety at all times. - Medication Management
In some cases, medications may be used to alleviate withdrawal symptoms, such as severe anxiety, depression, or other mental health issues that arise during detox. Medical professionals can administer these medications safely and adjust dosages as needed to help ease the discomfort associated with withdrawal. - Emotional Support
Detox can be a profoundly isolating experience, and having a supportive team can make a significant difference. Staff at detox centers are trained to provide not only medical support but also psychological encouragement throughout the detox process. This support can help individuals cope with the emotional stress of withdrawal and prepare them for the next steps in treatment. - Relapse Prevention
One of the biggest risks during the detox phase is the strong urge to use meth again to relieve withdrawal symptoms. Being in a supervised setting helps prevent relapse during this vulnerable time, as access to meth is restricted and immediate help is available to manage cravings.
Take the First Step Toward Recovery With Lumina Recovery
By understanding the symptoms and timeline of withdrawal, recognizing the importance of supervised detox, and engaging in comprehensive treatment programs, individuals can make significant strides towards recovery. This journey requires courage, support, and the right resources.
Lumina Recovery’s meth addiction program is equipped to provide supervised detox and medication-assisted treatment (MAT) at our treatment centers for those ready to take that step. If you or a loved one needs support for methamphetamine addiction or another substance use disorder, it’s crucial to seek help immediately.
Contact us today and start your journey to recovery and a healthier life.
Source:

Recognizing Signs of Meth Addiction
Methamphetamine, commonly known as meth and crystal meth, is a powerful and highly addictive substance that stimulates the central nervous system. Its misuse continues to be a grave issue in the United States with its potent impact and quick dependency.1 The threat posed by meth exceeds even that of opioids in some parts of the country, notably contributing to the rise in violent crimes.2
Meth addiction statistics from the 2021 National Survey on Drug Use and Health revealed that over 16.8 million Americans aged 12 and older have tried meth at least once in their lives, representing 6% of the population. In 2021 alone, approximately 2.5 million Americans reported using meth in the past year, underscoring its status as one of the country’s most commonly abused stimulants.2
This is why it is vital to recognize the signs and symptoms of meth addiction early. Whether you’re concerned about a loved one or seeking information for yourself, understanding these signals can be the first step towards seeking help and recovery.
Signs and Symptoms of Methamphetamine Abuse
Methamphetamine impacts both the mind and body profoundly, leading to a variety of symptoms that can affect every aspect of an individual’s life and indicate that they are abusing meth. Understanding the physical and psychological effects of meth use is critical in recognizing this dangerous substance use disorder.
Psychological Effects
Meth abuse dramatically alters brain chemistry, particularly affecting dopamine levels, which significantly influences mood and behavior. Some of the key psychological effects of meth addiction include:3
- Confusion and Disorientation: Users often experience difficulty in concentrating and organizing thoughts.
- Dependency for Pleasure: There is a marked loss of ability to feel pleasure without the drug, leading to increased dependency.
- Mood Disturbances: Users frequently exhibit mood swings, irritability, anger, and even severe depression, which can escalate to suicidal thoughts or attempts.
- Anxiety and Paranoia: These symptoms can range from general anxiety to full-blown panic disorders and paranoid delusions.
- Sleep Disturbances: Insomnia and extreme fatigue are common, disrupting normal sleep patterns.
- Hallucinations: Both tactile and auditory hallucinations may occur, often causing distress and dangerous reactions.
- Violent Behavior: Episodes of sudden and severe violence can appear, especially under the influence.
- Cognitive Decline: Chronic use can lead to severe memory loss, which may be permanent, and poor decision-making abilities due to altered brain function.
Physical Effects
The physical meth addiction signs are equally severe and often visibly noticeable:3
- Tremors and Weakness: A general physical shakiness and muscle weakness are common.
- Dry Mouth and Dental Issues: Users often suffer from ‘meth mouth,’ a condition marked by severe dental decay, gum disease, and teeth grinding due to decreased saliva and blood flow.
- Skin and Health Problems: Increased sweating, oily skin, and persistent sores from picking at the skin are telltale signs. These sores can lead to severe scarring.
- Weight Loss and Malnutrition: Significant weight loss and malnutrition occur due to decreased appetite and neglect of nutritional needs.
- Cardiovascular Issues: Irregular heartbeat, which can lead to sudden death, heart attacks, and chronic heart problems, are serious risks.
- Neurological Damage: Seizures and ‘tweaking,’ or uncontrollable repetitive movements, indicate severe neurological impairment.
- Organ Failure: Long-term use can cause kidney and liver failure, further complicating health conditions.

The Importance of Getting Professional Help for Methamphetamine Addiction
Methamphetamine addiction is a severe and often devastating condition that requires professional intervention. Due to the intense addictive properties of meth and its profound effects on both the brain and body, attempting to overcome this addiction without expert support can be dangerous and is often unsuccessful.
5 Reasons Why Professional Help Is Essential
- Meth withdrawal can be physically uncomfortable and psychologically challenging. Professional detox programs provide medical supervision which ensures safety, manages withdrawal symptoms, and reduces the risk of relapse.
- Addiction specialists can offer comprehensive treatment through a combination of therapies tailored to an individual’s needs. Meth rehab often includes behavioral therapy, counseling, and sometimes medication to help manage dependency.
- Given the strong link between meth use and mental health issues such as depression and anxiety, professional treatment programs also focus on mental health support through dual diagnosis treatment, which is crucial for a holistic recovery.
- Professionals can equip individuals with relapse prevention strategies and skills to handle cravings and triggers, which are critical for long-term abstinence.
- Treatment centers often help build strong support systems and networks, including peer support groups and family therapy, which are invaluable for recovery.
5 Ways to Seek Professional Help
- Speak with a healthcare provider, such as a doctor or mental health professional, who can provide an initial assessment and referral to addiction specialists.
- Contact local treatment facilities. Many centers offer comprehensive addiction treatment programs, including detox, inpatient, and outpatient options.
- Explore online resources and organizations to learn more about addiction and the various treatment options available. They also often provide directories of local and national treatment facilities.
- Consider support groups like Narcotics Anonymous to provide peer support, which is instrumental in maintaining sobriety. These groups can offer encouragement, understanding, and advice from others who have faced similar challenges.
- Involve loved ones like family and friends in the recovery process can provide additional emotional and motivational support which is vital during treatment.
Getting professional help for meth addiction not only increases the likelihood of successful recovery but also supports the individual’s overall well-being and return to a healthier lifestyle.
The journey to recovery is challenging but with the right professional guidance, it is achievable, leading to restored health and improved quality of life.
Take the First Step Towards Sobriety With Lumina Recovery
Understanding and recognizing the signs of meth addiction can empower you or your loved one to take the necessary steps toward recovery. Addiction is a formidable enemy, but with the right tools and support, victory is possible.
Lumina Recovery’s meth addiction treatment program provides support for anyone needing help on their path to sobriety. Whether you or a loved one needs detox, dual diagnosis care, or sober living, we are ready to help.
Reach out now to begin your journey to a healthier, meth-free life.
Sources:

Morphine Withdrawal Timeline and Detox
Morphine, a powerful opioid painkiller, is often prescribed to manage severe pain conditions. However, its use comes with a high risk of dependency and addiction. When individuals dependent on morphine decide to stop using the drug, they face a challenging withdrawal process.
Understanding the timeline and symptoms of morphine withdrawal is crucial for those preparing to discontinue use and for their loved ones supporting them through this journey. Our goal is to equip you with knowledge and understanding of what to expect during morphine withdrawal, including the physical and emotional symptoms and the importance of supervised detoxification.
Timeline and Symptoms of Morphine Withdrawal
How long do morphine withdrawal symptoms last? Morphine withdrawal effects can vary significantly among individuals, influenced by factors such as dosage, duration of use, method of consumption, and personal health history:1
Initial Symptoms (6-24 hours after last dose): Onset and Early Signs
- As the effect of morphine diminishes, anxiety levels can increase significantly, often leading to panic attacks or general unrest.
- The body begins to feel pain more acutely without morphine’s analgesic effects. Muscle aches are common and can be severe.
- Individuals may feel irritable and have a low tolerance for stressors.
- Sweating and runny nose are typical physical signs of withdrawal as the body starts to react to the lack of opioid stimulation.
- Excessive tearing and yawning are reflexive responses to the changes in the body’s neurochemical systems.
- Despite feeling extremely tired, many find themselves suffering from insomnia and difficulties sleeping due to discomfort and anxiety.
Peak Symptoms (1-3 days): Intensification of Discomfort
- Nausea, vomiting, diarrhea, and abdominal cramps are common as the gastrointestinal tract reacts to the absence of opioids.
- Dilated pupils and visual disturbances are a direct consequence of neurological changes.
- Goosebumps and chills reflect the body’s thermoregulatory response to withdrawal.
- The cardiovascular system can become overactive, leading to rapid heart rate and high blood pressure.
Subsiding Symptoms (4-10 days): Gradual Easing of Acute Symptoms
- Nausea, vomiting, and diarrhea begin to subside, and appetite may start to return.
- As the body recalibrates, the severity of muscle aches
- Although mood swings and irritability may persist, there is generally an improvement in overall emotional state.
Post-Acute Withdrawal Syndrome (Months): Long-Term Recovery Challenges
- People who stop taking morphine may start feeling post-acute withdrawal syndrome (PAWS) about 6 to 9 weeks later. These symptoms can last for months after stopping the drug.
- Depression and anxiety can linger or reemerge, particularly during stressful periods.
- Cravings for morphine can occur suddenly and be intense, particularly in response to triggers.
- Problems with memory, concentration, and decision-making can persist, affecting daily functioning.
- Insomnia and altered sleep patterns may continue, requiring management strategies.2
Managing Symptoms With Supervised Detox
Supervised detoxification is a critical step in the management of morphine withdrawal symptoms. It involves medical oversight in a controlled environment, ensuring safety and comfort while the body clears itself of opioids.
This process is designed to minimize the risks associated with withdrawal and to support the individual through the acute phases of morphine detox.
Benefits of Supervised Detox
- Medical Monitoring: One of the primary benefits of a supervised detox is constant medical monitoring. Health professionals track vital signs, manage withdrawal symptoms, and address any complications that arise, thereby preventing potential health risks such as dehydration, seizures, or severe metabolic disturbances.
- Medication-Assisted Treatment (MAT): Medications can play a significant role in easing withdrawal symptoms and cravings. Medications like buprenorphine or methadone can help the body adjust to not having morphine, making symptoms less severe. Other medications, such as clonidine, are used to address issues like anxiety and high blood pressure.
- Psychological Support: Detox often includes support for psychological symptoms. Anxiety, depression, and other mental health challenges that arise during detox can be addressed through counseling and therapy. This support is crucial in helping individuals understand and cope with the emotional aspects of opioid withdrawal.
- Relapse Prevention: By detoxing in a supervised setting, individuals are less likely to use opioids again to relieve their withdrawal symptoms. This controlled environment reduces the risk of relapse during a highly vulnerable period.
Components of a Supervised Detox Program
- Assessment: Upon entry into a detox program, a comprehensive assessment is conducted to determine the physical and psychological state of the individual. This assessment helps in creating a personalized detox plan.
- Stabilization: The next step is stabilization, which involves the use of medications and therapy to manage withdrawal symptoms effectively. The goal is to reach a state where the individual is physically stable and fully prepared for ongoing treatment.
- Preparation for Further Treatment: Detox is only the first step in addiction treatment. During detox, staff will help people get ready for the next steps in their recovery, such as entering rehabilitation programs. Education about addiction and counseling are integral parts of preparing individuals for life after detox.

Importance of Continuity in Care
Continuity in care is important for recovering from morphine addiction, connecting initial detox with long-term sobriety. This sustained, ongoing treatment approach ensures that the gains made during detoxification are not lost but are instead reinforced through further therapeutic interventions and support systems.
Continuity in care helps prevent relapse by smoothly moving patients from detox to rehab to outpatient support. It also addresses psychological issues and promotes behavioral changes needed for recovery.
People can create a safe place to recover from opioid addiction. They can learn new coping strategies and build a support system. Addiction experts, who understand the challenges of recovery, can help them along the way.
Seek Professional Help for Morphine Addiction With Lumina Recovery
Understanding the withdrawal timeline and symptoms prepares individuals and their families for the journey ahead and highlights the importance of professional medical supervision.
Lumina Recovery offers medically assisted detox and treatment programs for morphine and opioids that are customized to meet individual needs. If you or someone you love is struggling with morphine dependency, remember that you are not alone.
Take control of your future and contact us today to start your journey towards a life free from addiction.
Sources:
Morphine Addiction: Recognizing Signs and Symptoms
Morphine is an opioid medication used to manage severe pain, typically prescribed after surgery or for serious health conditions. However, its effectiveness comes with a high risk of opioid use disorder.
Morphine addiction can disrupt lives, damage relationships, and lead to significant health complications. Understanding the signs and symptoms of addiction is crucial for early intervention and effective treatment.
What Is Morphine?
Morphine is derived from the opium poppy and is one of the most effective painkillers available in modern medicine. It works by binding to the body’s opioid receptors in the central nervous system, blocking pain and often inducing feelings of euphoria.
This combination of pain relief and pleasure can lead to psychological dependence and physical addiction. For someone in pain or for those around them, recognizing the difference between necessary medical use and problematic abuse can be challenging.1
Recognizing the Signs of Morphine Addiction
Understanding the signs of morphine dependence is crucial for timely intervention. By recognizing both subtle and overt changes in physical and behavioral well-being, individuals can identify potential addiction early, enabling quicker and more effective treatment.
Physical Symptoms
Physical symptoms and side effects of morphine addiction are often the most visible and measurable indicators. These symptoms reflect how the body reacts to the presence and absence of the drug, providing key insights into the physical dependence that has developed.
- Drowsiness and Sedation: Excessive sleepiness and a general lethargic state that interferes with daily activities.
- Gastrointestinal Issues: Persistent stomach pain, cramps, nausea, and constipation, which are direct effects of opioid use.
- Dry Mouth and Headaches: Frequent discomforts such as dry mouth and persistent headaches.
- Small Pupils: Constricted pupils, often noticeable in various lighting conditions.
- Respiratory Depression: Shallow, slow breathing which can be life-threatening, often a result of high doses.
- Skin Changes: Blue or purple coloration of the skin indicating possible circulatory or oxygenation issues.
- Neurological Symptoms: Hallucinations, severe agitation, muscle twitching, and loss of coordination are severe and require immediate medical attention.
- Cardiovascular Issues: Irregular heartbeats or chest pain, particularly dangerous and potentially indicative of overdose.2
Behavioral Signs
Behavioral signs and symptoms of morphine abuse are changes in actions and lifestyle that may signal a problem. These behaviors often result from the psychological effects of addiction and the individual’s efforts to maintain their access to the drug.
- Doctor Shopping: This involves seeking prescriptions from multiple healthcare providers to obtain more of the medication, often under the pretenses of lost prescriptions or inadequate pain relief.
- Social Withdrawal: Withdrawal from social activities and isolation from friends and family are common as the individual may spend more time using or obtaining the drug.
- Secrecy and Deception: Individuals may lie about their drug use, the amount consumed, or methods of obtaining more, including hiding morphine or denying there is a problem.
- Mood Swings: Rapid and inexplicable changes in mood, ranging from euphoria when the drug is accessible to depression or irritability when it is not, are typical.
- Financial Problems: Uncharacteristic borrowing of money, selling possessions, or even stealing to fund the drug habit are signs that often emerge as the addiction progresses.
By understanding these expanded signs of morphine addiction, individuals and their loved ones can be better equipped to recognize the need for professional help. Early detection is key to managing the addiction effectively and moving towards recovery.
Risk Factors for Morphine Addiction
Morphine addiction often develops due to a combination of genetic, environmental, and personal factors. Understanding these risk factors can help in identifying vulnerabilities and implementing preventive measures:
- Genetic predispositions can play a role in addiction. Individuals with a family history of substance abuse are more likely to develop similar issues.
- Individuals suffering from mental health disorders, such as depression, anxiety, or post-traumatic stress disorder (PTSD), are at a higher risk of addiction, often using morphine to self-medicate.
- Chronic use of morphine, even when prescribed for legitimate medical reasons, increases the risk of dependency. The body’s tolerance to the drug escalates, necessitating higher doses for the same effect.
- A social environment that is supportive can deter drug use, whereas a stressful or enabling environment can increase the risk.
- Early use of opioids at a young age can influence brain development, increasing the likelihood of developing addictive behaviors later in life.
- Lack of knowledge about morphine’s addictive potential and the dangers of long-term use may lead individuals to misuse the drug.3

The Importance of Getting Help
Recognizing the need for help and taking the first step toward recovery is crucial in dealing with morphine addiction. Here’s why seeking help is vital:
Long-term use of morphine can lead to severe health issues, including respiratory depression, cognitive impairment, and potential overdose. Medical professionals can help prevent these outcomes.
Addiction can strain relationships with family members, friends, and colleagues. Rehabilitation and evidence-based therapy can help in rebuilding these bonds and improving social support, which is essential for recovery.
Addiction can consume an individual’s life, leading to a loss of productivity and a decline in overall well-being. Treatment under medical supervision helps individuals regain control and work towards a fulfilling life.
Addiction treatment centers provide comprehensive recovery programs, including detoxification, therapy, and support groups for morphine addiction treatment.
Seeking help can also avert potential legal issues related to drug acquisition and use, and help stabilize financial situations by stopping the high costs associated with obtaining the drug illicitly.
Take the First Step Towards Sobriety With Lumina Recovery
Understanding the signs, symptoms, and risk factors of morphine addiction is the first step toward addressing this challenging condition. If you or someone you love is showing signs of addiction, it’s crucial to acknowledge the problem and seek professional help.
At Lumina Recovery, we provide initial detoxification, dual diagnosis, therapy services, and more for those needing morphine addiction treatment.
Reach out for help today and start your journey to recovery to regain control of your life.
Sources:

Fentanyl Withdrawal Timeline: Understanding the Process
Fentanyl is a synthetic opioid that is 50 to 100 times more potent than morphine. It is often prescribed for severe pain management but has gained notoriety due to its misuse and highly addictive properties.1
Understanding fentanyl withdrawal is a critical step toward recovery, as navigating the process safely and effectively can improve the chances of long-term sobriety.
What Is Fentanyl?
Fentanyl was first developed as a pain-relieving medication. In medical settings, it is used for post-surgical pain or chronic pain in cancer patients.
However, illicit fentanyl—often mixed with other drugs—has fueled the opioid and fentanyl crisis in America. Its potency makes it highly addictive, even after short-term use, increasing the risk of overdose and dependency. Many users are unaware of the fentanyl content in substances they consume, contributing to a rapid rise in substance abuse rates and accidental overdoses.
While prescription fentanyl is carefully regulated, street versions are frequently mixed with other opioids, creating dangerous combinations that further increase dependency. Recognizing fentanyl addiction early can help prevent severe complications and support a structured recovery plan.
Why Does Fentanyl Withdrawal Occur?
Withdrawal occurs when the body adapts to the constant presence of fentanyl. Over time, users develop a tolerance, requiring higher doses to achieve the same effects. This dependence results in physical and psychological symptoms when fentanyl use stops.
Fentanyl binds to opioid receptors in the brain, altering pain perception and triggering dopamine release. When use is discontinued, the brain struggles to regain balance, leading to withdrawal symptoms. The severity of these symptoms often discourages individuals from quitting without medical assistance, making professional support a key component of successful recovery.
Fentanyl Withdrawal Symptoms
Symptoms of fentanyl withdrawal can manifest physically and psychologically, which can be uncomfortable and dangerous. The severity and duration of opioid withdrawal symptoms often depend on the duration of use, the amount used, and individual health factors:1
- Muscle and Joint Pains: These can be severe and feel similar to a bad flu.
- Gastrointestinal Distress: This includes nausea, vomiting, diarrhea, and stomach cramps, which are common and particularly discomforting.
- Cold Flashes With Goosebumps: These symptoms can be accompanied by uncontrollable shivering.
- Sweating: Excessive sweating is typical, regardless of the temperature or physical activity levels.
- Uncontrollable Leg Movements: Known as “restless legs syndrome” in some contexts, this symptom involves involuntary leg twitches and jerks that can make it difficult to rest or sleep during withdrawal.
- Insomnia and Sleep Disturbances: Difficulty falling asleep, staying asleep, or experiencing restful sleep is common.
- Cravings: Intense cravings for fentanyl are one of the most challenging aspects of withdrawal, often leading to relapse if not properly managed.
Fentanyl Withdrawal Timeline
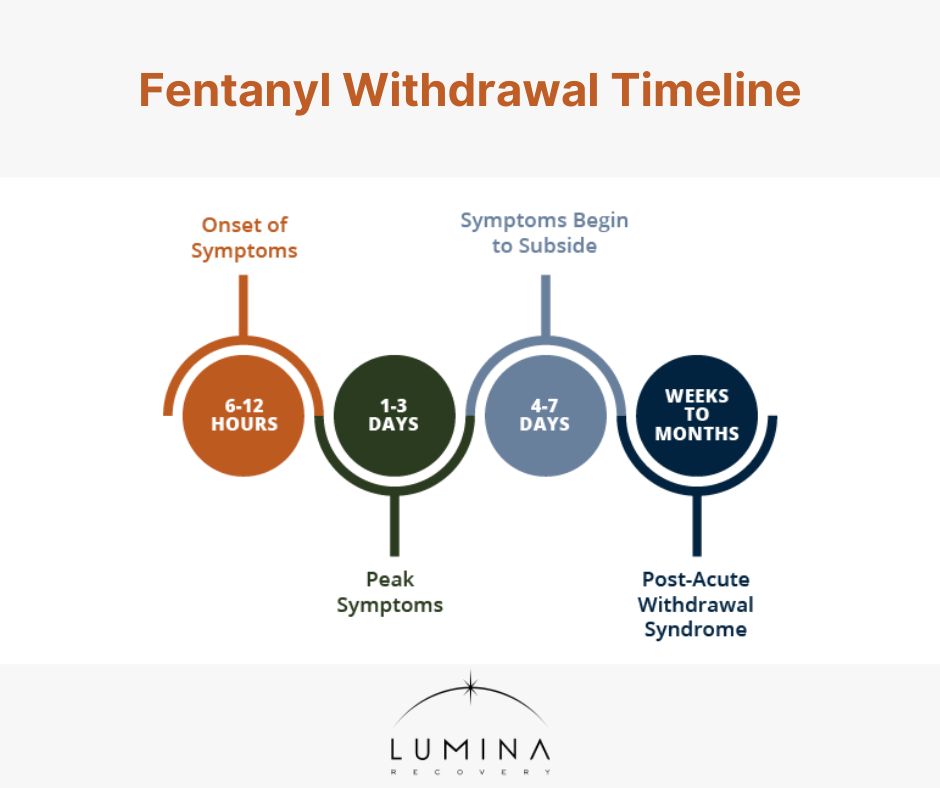
The withdrawal from fentanyl is a multi-stage process, each stage characterized by various symptoms. Understanding the fentanyl withdrawal symptoms timeline is essential for anyone facing recovery from fentanyl dependency. The timeline can vary but typically follows this pattern:2
Stage 1: Onset of Symptoms (6-12 hours)
Symptoms start mild and gradually increase in severity. These include muscle aches, anxiety, and a strong craving to use the drug.
Stage 2: Peak Symptoms (1-3 days)
This is when symptoms are at their worst. Physical symptoms such as nausea, vomiting, diarrhea, and severe muscle aches are common. Psychological symptoms such as anxiety, depression, and intense cravings also peak during this time.
Stage 3: Symptoms Begin to Subside (4-7 days)
Physical symptoms start to lessen in intensity, but psychological symptoms like depression and cravings may persist. This is a critical period where support is essential to reduce the risk of relapse.
Post-Acute Withdrawal Syndrome (Weeks to Months)
Some symptoms, particularly psychological ones like mood swings, anxiety, and ongoing executive dysfunction can persist for weeks or months after the initial withdrawal period.
Post-acute withdrawal syndrome (PAWS) can make long-term sobriety challenging and requires continued support and possibly ongoing therapy.3
Factors That Affect Withdrawal
Several factors influence the severity and duration of withdrawal:
- Dosage and Duration: Higher doses and longer use result in more intense withdrawal.
- Individual Health: Age, metabolism, and overall health impact recovery.
- Co-occurring Conditions: Mental health issues or other substance use disorders can complicate withdrawal.
- Support System: Individuals with family or professional support often experience better outcomes.
- Environment: A stress-free, supportive setting can promote recovery.

Coping With Withdrawal Symptoms
Managing withdrawal symptoms effectively is a vital part of the recovery process. Developing both short-term and long-term coping tools can provide the support needed to navigate this challenging time successfully.
Short-Term Coping Strategies
- Stay hydrated and eat nutritious foods to maintain energy.
- Get plenty of rest and engage in light exercise to boost endorphins.
- Practice relaxation techniques like meditation and deep breathing to reduce anxiety.
Long-Term Coping Tools
- Attend therapy and support group meetings to stay accountable.
- Develop relapse prevention strategies, such as identifying triggers and learning new habits.
- Build healthy routines, including regular exercise and stress management techniques, to support emotional well-being.
Fentanyl Detox and Treatment Options
Fentanyl detox is a critical step in addiction treatment to this powerful opioid. Because fentanyl is highly addictive and withdrawal symptoms can be severe, medically supervised detox programs are often the safest and most effective approach.
Medical Detox
Supervised detox programs offer a safe environment where symptoms are managed with medications and professional care. Monitoring ensures that patients stay hydrated, receive proper nutrition, and avoid dangerous complications.
Medication-Assisted Treatment (MAT)
Medications such as naltrexone, methadone, and buprenorphine are used to reduce cravings and manage withdrawal symptoms. These treatments support long-term recovery by stabilizing brain chemistry and easing physical dependence.
Therapies and Counseling
Many outpatient and inpatient rehabs use cognitive behavioral therapy (CBT) and group therapy to address the psychological aspects of addiction, which promote long-term recovery. Individual therapy sessions can help uncover underlying triggers and build coping strategies.
Frequently Asked Questions (FAQs)
1. How long does it take for fentanyl to leave your system?
Fentanyl typically leaves the system within 24–72 hours, but withdrawal symptoms can last longer.
2. How long do fentanyl withdrawals last?
Acute withdrawal symptoms generally last 1–2 weeks, while psychological symptoms can persist for months.
3. What is one of the first signs of withdrawal?
Anxiety and restlessness often appear first, signaling the onset of withdrawal.
Find Long-Term Recovery With Lumina Recovery
Fentanyl withdrawal can be overwhelming, but understanding the symptoms and fentanyl withdrawal timeline is the first step to a healthier life. With the right support, recovery is possible.
Lumina Recovery’s treatment centers offer medical detox to help manage fentanyl withdrawal symptoms safely and medication-assisted treatment (MAT) to reduce cravings and promote long-term success.
If you or a loved one is struggling with fentanyl addiction or an opioid use disorder, contact Lumina Recovery today to learn about our customized treatment plans.
Sources:

Fentanyl Addiction Signs and Symptoms
Despite fentanyl’s legitimate medical use for severe pain, such as in advanced cancer patients, addiction to fentanyl is a critical and growing issue in communities across the globe.
As a synthetic opioid that is 50 to 100 times stronger than morphine, potential for addiction and overdose on fentanyl is very high. Its potency can make it difficult for users to gauge how much they are consuming, potentially leading to fatal consequences.1
It is extremely important to be educated on the key signs and symptoms of addiction, and understanding the importance of seeking professional help is crucial for both individuals struggling with fentanyl abuse and their concerned loved ones.
Key Signs and Symptoms of Fentanyl Addiction
Knowing the symptoms and signs of fentanyl use is vital for early detection and intervention. Fentanyl use disorder can rapidly lead to physical dependency and profound psychological changes.
Recognizing the most common physical and behavioral indicators and side effects that may suggest a person is struggling with drug abuse can help in seeking timely support and treatment.
Physical Signs
- Changes in sleep patterns and disrupted sleep are common, with individuals either suffering from insomnia or finding themselves excessively sleepy.
- Noticeable weight loss without a clear reason is often seen due to reduced appetite.
- Persistent flu-like symptoms including sweating, shaking, and gastrointestinal distress such as nausea and vomiting can occur.
- Constricted “pinned” pupils even in dim lighting can be noticeable.
- Seizures can have a severe physical effect and need immediate medical attention.
Behavioral Signs
- Individuals may withdraw from social interactions and become secretive about their whereabouts and activities.
- Failing responsibilities in all aspects of life including personal, professional, or educational can occur.
- Increased engagement in risky behaviors are common, such as driving under the influence or using non-sterile needles.
- Sudden or worsening financial difficulties may be a result of spending substantial amounts of money on the substance.
- Some people may doctor shop by seeking prescriptions from multiple healthcare providers in an effort to maintain their supply.
- Rapid and extreme mood swings can occur, especially as the effects of the drug wear off.
- Anxiety and paranoia can escalate with the use of fentanyl, affecting the person’s mental health and quality of life.2
Effects of Fentanyl Addiction
Regular use of fentanyl can cause mood instability, leading to unpredictable emotional responses and complicating personal and professional relationships.
Physiological effects include reduced libido and significant digestive issues such as constipation, which can become chronic and debilitating. Women may experience menstrual problems, further affecting their overall health.
A particularly severe consequence of regular fentanyl use is respiratory impairment. This condition can severely diminish lung function, increasing the risk of respiratory failure, especially during overdose situations.
Moreover, regular fentanyl use typically leads to both dependence and tolerance. Dependence, or addiction, means that an individual will feel unable to function normally without the drug, leading to compulsive drug-seeking behavior.
Tolerance develops simultaneously, compelling the user to consume increasingly larger doses to achieve the same effects previously obtained with smaller amounts. Together, these factors create a dangerous cycle that escalates the risk of overdose and complicates recovery efforts.3

The Importance of Getting Help
Addressing fentanyl addiction and opioid use disorder is imperative due to the high risk of overdose and severe health complications associated with its use. Fentanyl is incredibly potent, and even small amounts can lead to overdose and death. This danger underscores the importance of recognizing addiction signs early and seeking professional help immediately.
Treatment for fentanyl addiction involves stopping drug use and comprehensive medical and psychological support to address the underlying issues that contribute to addiction. Professional treatment can provide the tools and strategies necessary for long-term recovery, including relapse prevention. Addiction also often affects not just the individual but also their family members and friends, making community support and family counseling integral components of effective treatment.
6 Steps to Get Help for Fentanyl Addiction
If you or someone you know is struggling with fentanyl addiction, taking the step to get help can be daunting but is crucial for recovery.
- Acknowledge the problem. The first step in seeking help is recognizing and admitting the presence of a substance use disorder.
- Consult a healthcare professional. Speak with a doctor or addiction specialist who can assess the situation and recommend treatment options. This might include detoxification, medication-assisted treatment, and therapy.
- Contact addiction treatment centers. Facilities like Lumina Recovery specialize in providing comprehensive fentanyl treatment programs tailored to individual needs. These programs typically include medical detox, counseling, therapy, and support groups.
- Involve loved ones. Having the support of family and friends can be a powerful motivator during recovery. Consider involving them in the treatment process through family therapy or education programs.
- Explore support groups. Organizations such as Narcotics Anonymous (NA) or SMART Recovery offer community support and resources for individuals dealing with substance abuse.
- Plan for long-term recovery. Recovery from addiction is a long-term process that may require ongoing support. Planning for long-term strategies, such as continued therapy or maintenance medication, can help sustain sobriety.
Seek Help and Start Your Sobriety With Lumina Recovery
Recognizing the signs and understanding the risks associated with fentanyl use are crucial steps toward addressing this crisis. For those struggling with addiction or for loved ones witnessing these struggles, it’s vital to seek professional help.
Lumina Recovery provides the necessary support and resources for opioid and fentanyl addiction treatment. This may start with medication-assisted treatment (MAT) to manage withdrawal symptoms and extend to dual diagnosis services to treat the root cause. Let this be the moment of change towards a healthier, drug-free life.
If you or someone you care about is struggling with fentanyl addiction, don’t wait. Reach out for help today and begin the journey towards a healthier, drug-free future.
Sources:

Should You Choose Outpatient Treatment, Sober Living, or Both Options?
Combining outpatient treatment with sober living can be an effective approach. It offers the flexibility of outpatient care alongside the supportive structure of a sober living home (SLH). This combination allows you to immerse yourself in a recovery-focused community while still attending therapy and other outpatient services. It’s an excellent choice if you need additional support or are transitioning from a more intensive inpatient program.
Outpatient treatment provides a structured recovery program while allowing you to live at home or in a supportive environment of your choosing. This flexibility is ideal for those who need to balance treatment with work, school, or family commitments. Outpatient programs, such as a partial hospitalization program (PHP) or intensive outpatient program (IOP), vary in intensity, allowing you to choose one that fits your schedule and recovery needs.
Sober living provides a supportive, drug- and alcohol-free environment. It fosters a sense of community and accountability, which is crucial in early recovery. Sober living houses offer a stable space to build relationships with others on the same journey, reinforcing your commitment to sobriety.
Deciding What’s Right for You
Choosing between outpatient rehab, sober living, or a combination of both depends on your specific needs. To help guide your decision, consider these questions:
- Do you need a supportive community to help maintain your sobriety?
- Is your home environment stable and conducive to recovery?
- Would a structured living situation help you stay on track?
- Can you balance other responsibilities while in treatment?
Ultimately, the right choice comes from consulting with healthcare professionals and addiction specialists to find the treatment plan that best suits your individual needs.
Who Is a Good Candidate for Outpatient Treatment?
Outpatient rehab is ideal for individuals who:
- Have stabilized during inpatient treatment and made significant progress in their recovery.
- Have a supportive home environment with family members or friends who encourage sobriety and provide emotional support.
- Can balance other responsibilities while attending therapy sessions and group meetings.
- Are motivated to engage in their recovery and committed to sobriety.
- Have a lower risk of relapse and can benefit from continued treatment without full-time supervision.
Outpatient rehab is most effective when individuals are purposeful and focused. It’s designed for those who can attend sessions regularly, follow their treatment plans, and actively work toward sobriety. This approach allows you to take control of your journey.
Individuals with co-occurring mental health disorders such as depression, anxiety, or PTSD can also benefit from outpatient treatment, as it addresses both addiction and mental health simultaneously.
Candidates who understand the importance of relapse prevention strategies and are dedicated to implementing them are ideal for these programs, which focus on teaching coping skills and preventing relapse.
A thorough assessment by addiction professionals is crucial to determine the most appropriate treatment path for each individual.
Who Is a Good Candidate for Sober Living?
Sober living houses are suited for those who:
- Are currently in or have completed an addiction treatment program. This foundation ensures they have acquired essential coping skills and are ready for the next phase of recovery.
- Need a supportive and structured environment to maintain sobriety.
- Are transitioning from inpatient rehab or outpatient treatment and want a bridge to independent living.
- Thrive in a community-oriented setting with accountability and peer support.
- Are willing to follow house rules, attend meetings, and contribute to the community.
- Benefit from a stable environment that helps reduce the risk of relapse.
The ideal candidate for a sober living house possesses qualities that align with the goals of maintaining sobriety and fostering a supportive community.
They display a willingness to actively participate in a residential recovery program and recognize the importance of continued support and structure.
An ideal resident has sufficient coping skills to live semi-independently. These skills include managing cravings, handling stress, and making healthy choices.
Remember, every person’s situation is unique, and a thorough assessment by addiction professionals helps determine the suitability of a sober living house for your recovery journey.

Who Is a Good Candidate for Both Options?
Combining sober living with outpatient rehab is ideal for individuals who meet the following criteria:
- Those transitioning from a more intensive inpatient residential program to outpatient treatment who need a supportive environment to continue their recovery journey.
- People committed to sobriety who understand the value of a drug- and alcohol-free environment while working on their recovery through outpatient services.
- Individuals who benefit from a stable, structured living situation that provides peer support, accountability, and a sense of community with others in recovery.
- Those who are willing to follow SLH rules, such as curfews, group meetings, and drug testing, as part of their commitment to recovery.
- People who understand the importance of relapse prevention and are actively engaged in learning coping skills, attending support groups, and participating in therapy sessions.
- Individuals with co-occurring mental health disorders may benefit from outpatient treatment to address both their substance use and mental health needs while residing in the stable environment of a SLH.
If you’re considering combining sober living with outpatient treatment, it’s crucial to have a thorough assessment by addiction professionals to ensure this approach suits your unique needs. Ultimately, the best recovery path is the one that aligns with your personal circumstances and goals. Reach out to a professional treatment center or addiction specialists for personalized advice.
Why Choose Lumina Recovery?
Our caring team at Lumina Recovery is here to evaluate your situation and suggest the best treatment plan tailored to your unique needs and history. We are dedicated to creating a recovery plan that aligns with your individual requirements, offering you the best chance at lasting recovery.
Our drug and alcohol rehab programs are staffed with addiction specialists, individual therapists, and holistic therapy providers who collaborate to create comprehensive treatment plans.
If you’d like to learn more about our integrated recovery options and discuss which approach might be best for you, please reach out to the Lumina Recovery team.
We’re here to help you make the right choice for your journey towards sobriety and wellness. You have our full support, and you are not alone on this journey.

Vicodin Withdrawal: Symptoms and What to Expect
Vicodin, a commonly prescribed painkiller combining hydrocodone and acetaminophen, is effective for pain management but carries a significant risk of misuse and addiction. Over time, repeated use of Vicodin can lead to physical dependence and addiction, leading to withdrawal symptoms when the drug use is discontinued.
Understanding Vicodin withdrawal symptoms, the process of detoxification, and the treatment options available are critical for individuals struggling with addiction and their loved ones. Let’s explore the signs and symptoms of Vicodin dependence, the Vicodin withdrawal timeline, the challenges of detox, and the support systems that make recovery possible.
Statistics About Vicodin Use and Abuse
The misuse of prescription opioids, like Vicodin, remains a significant concern in the United States. In 2023, approximately 8.6 million Americans aged 12 and older admitted to misusing prescription opioids within the past year. Among them, over 5 million individuals reported struggling with a prescription use disorder during the same period.1
These alarming numbers underscore the prevalence of Vicodin abuse and other opioid misuse, emphasizing the urgent need for awareness, prevention, and accessible treatment options to combat this growing crisis
What Is Vicodin Withdrawal?
Withdrawal occurs when someone dependent on Vicodin stops or significantly reduces their use. Prolonged Vicodin use alters the brain’s neurotransmitter balance, creating physical and psychological reliance on the drug. When the brain no longer receives Vicodin, withdrawal symptoms set in as the body struggles to regain balance.
Factors Influencing Opioid Withdrawal Severity
- Duration of Use: Prolonged use increases the intensity of Vicodin withdrawal symptoms.
- Dosage: Higher doses of medication amplify hydrocodone withdrawal.
- Health Conditions: Underlying medical or mental health issues can worsen withdrawal.
- Co-Occurring Substance Use: Individuals using multiple substances may experience more severe symptoms.
Expected Symptoms of Vicodin Withdrawal
Withdrawal symptoms of Vicodin addiction can range widely in intensity and duration based on individual factors such as duration of use, higher dose, and the person’s general physical and mental health.2
Physical Symptoms
- Muscle Aches and Joint Pain: Often described as flu-like symptoms, these can range from mild to extremely debilitating.
- Gastrointestinal Distress: This includes nausea, vomiting, diarrhea, and stomach cramps, which are common and can lead to dehydration and nutrient depletion.
- Temperature Regulation Issues: Many experience chills, sweats, and goosebumps as the body struggles to manage its temperature without the influence of Vicodin.
- Increased Heart Rate and Blood Pressure: These symptoms can be particularly dangerous for those with underlying heart conditions.
- Fatigue and Exhaustion: Despite feeling very tired, many people find it difficult to sleep properly during withdrawal.
Psychological Symptoms
- Anxiety and Depression: Withdrawal can exacerbate underlying mental health conditions or trigger new ones.
- Irritability and Mood Swings: Emotional regulation becomes more difficult, leading to sudden changes in mood.
- Cravings: The desire to use Vicodin can be strong and persistent, often triggered by both physical discomfort and psychological stress.
- Disorientation and Confusion: Some individuals may experience a lack of focus or confusion during withdrawal.
- Insomnia and Disturbed Sleep Patterns: Difficulty falling asleep, staying asleep, or experiencing restorative sleep is common.
Vicodin Withdrawal Timeline
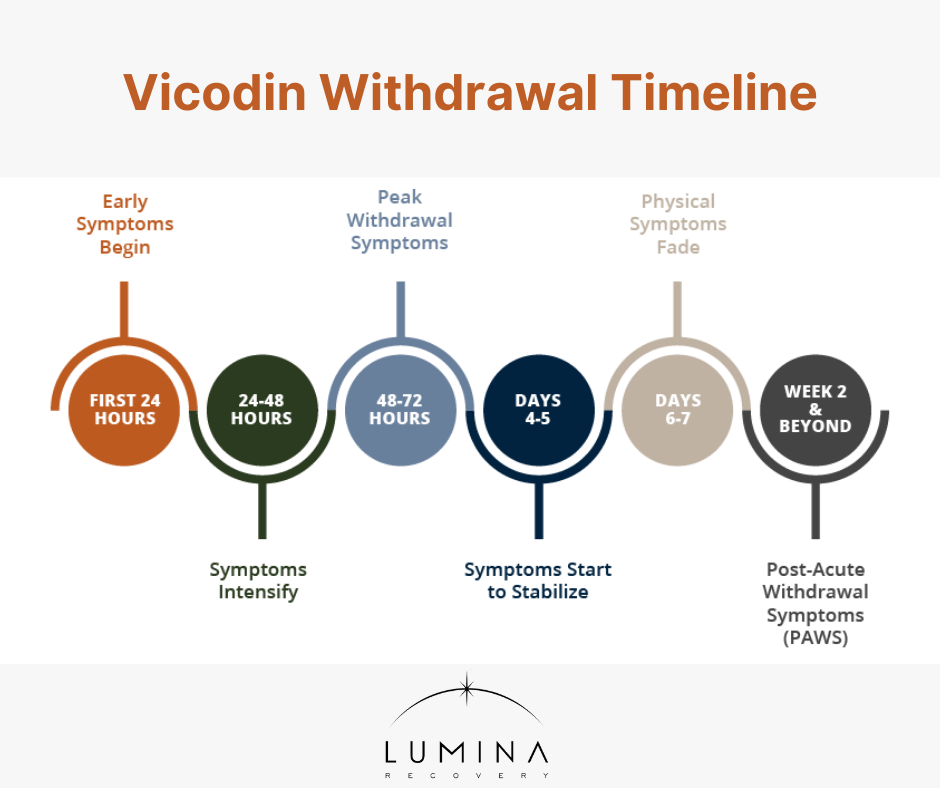
The withdrawal from hydrocodone timeline can be a challenging experience, with the amount of time the process takes significantly varying from person to person. It’s important to know the side effects and risk factors for Vicodin withdrawal that individuals might experience at different stages:3
First 24 Hours
- Early symptoms start to appear as the drug begins to leave the system.
- Symptoms may include restlessness, anxiety, muscle aches, and an intense craving for the drug.
- Mild symptoms such as excessive sweating, agitation, headaches, and a runny nose are also common.
24-48 Hours
- Symptoms may begin to intensify. This period can be particularly uncomfortable.
- Common symptoms include increased tearing, yawning, and sweating, as well as insomnia and irritability.
- Gastrointestinal distress may start to occur, manifesting as loss of appetite, stomach cramps, and nausea.
48-72 Hours
- This is often the peak of physical withdrawal symptoms.
- Symptoms can include diarrhea, vomiting, and continued nausea, along with peak levels of muscle aches and possibly abdominal cramping.
- Chills, tremors, and goosebumps are frequent, indicating the body’s struggle to regulate temperature and pain sensation.
Days 4-5
- Symptoms may remain intense but begin to stabilize. While still very uncomfortable, the body starts to adapt to the absence of the drug.
- Physical symptoms like nausea and muscle aches begin to decrease gradually.
- Psychological symptoms can become more pronounced, including anxiety, depression, and continued insomnia.
Days 6-7
- Physical symptoms generally start to subside significantly.
- Emotional and psychological symptoms may persist or increase, such as mood swings and irritability.
- Cravings for Vicodin can remain strong, posing a risk for relapse, particularly if psychological support is not in place.
Week 2 and Beyond
- Most severe physical symptoms should have subsided. However, some individuals might continue to experience extended withdrawal symptoms, referred to as post-acute withdrawal syndrome (PAWS).
- PAWS can include ongoing mood disturbances, fatigue, chronic pain, and irregular sleep patterns.4
- Mental illness support remains crucial, as psychological cravings and emotional instability can go on for weeks or even months after stopping Vicodin.
The hydrocodone withdrawal symptoms timeline mirrors that of Vicodin, as Vicodin contains hydrocodone and affects the brain in a similar way.

The Detox Process
Detox is the first critical step in overcoming addiction. Attempting to withdraw from Vicodin without professional help carries serious risks. A structured Vicodin detox ensures safety and reduces the discomfort associated with withdrawal.
Medical Detox vs. At-Home Detox
Unsupervised withdrawal can be dangerous, increasing the risk of relapse and severe symptoms. Medical detox provides professional monitoring, access to medications, and nutritional support to ease withdrawal.
Medications Used During Detox
Buprenorphine or methadone can help reduce cravings and withdrawal symptoms.
Over-the-counter medications, such as anti-nausea or anti-diarrheal drugs, help manage symptoms.
The Role of Hydration and Nutrition
Proper hydration and a balanced diet support the body’s recovery during detox, addressing physical symptoms like fatigue and nausea.
Treatment and Recovery Options
After detox, comprehensive treatment is necessary to address the root causes of addiction and prevent relapse.
- Inpatient programs offer 24/7 care in a controlled environment, ideal for those with severe addiction or co-occurring mental health disorders. This intensive approach includes therapy, counseling, and medical monitoring.
- Outpatient care, including therapy sessions and support groups, provides flexibility for those balancing work or family obligations.
- Therapies like cognitive behavioral therapy (CBT) and dialectical behavior therapy (DBT) help individuals manage cravings, address underlying issues, and develop coping mechanisms.
- Support groups like Alcoholics Anonymous (AA), Narcotics Anonymous (NA), or other community programs provide ongoing peer support, which is crucial for long-term sobriety.
Frequently Asked Questions (FAQs)
1. How long do Vicodin withdrawals last?
Symptoms typically last one to two weeks, though psychological effects may persist longer.
2. What is the first sign of Vicodin withdrawal?
Early symptoms include sweating, muscle aches, and irritability.
3. What reduces Vicodin withdrawal symptoms?
Medications like methadone, along with hydration and rest, can alleviate symptoms.
Take the First Step Toward Sobriety With Lumina Recovery
Vicodin withdrawal can feel overwhelming, but understanding the opiate withdrawal timeline and seeking professional support can make the journey manageable. The signs and symptoms of Vicodin addiction highlight the importance of structured detox and treatment.
At Lumina Recovery, we specialize in medically assisted detox, ensuring a safe and effective withdrawal process, and dual diagnosis treatment to address underlying mental health conditions that may accompany addiction. Our comprehensive approach builds a solid foundation for lasting recovery.
If you or a loved one is struggling with Vicodin addiction, contact us today to begin the journey toward a healthier, addiction-free life.
Sources:
Additional Resources
Once you have completed your rehabilitation program at one of our drug and alcohol treatment centers, you should try to surround yourself with people who can encourage you to stay sober. Many people find that support groups are the best source of encouragement. You can find hundreds of support groups and meetings in your community. Our drug addiction treatment centers stress the importance of personal chemical dependency resources, especially when you are new to sobriety. Below are various addiction and mental health resources for people in recovery who want additional support.
Christian Addiction Recovery Resources
Our substance abuse services aren’t limited to specific programs, but rather we believe in the importance of incorporating faith-based programs to promote spiritual healing, like our Faith in Recovery program.
With that said, below are some faith-based addiction recovery resources that could help you in your spiritual healing from addiction:
- Battlefield of the Mind by Joyce Meyer
- Boundaries by Dr. Henry Cloud & Dr. John Townsend
- Christian Families in Recovery: A Guide for Addiction, Recovery, and Intervention Using God’s Tools of Redemption by Robert and Stephanie Tucker
- Club New Life Christian Ministry for Addiction and Recovery
- Lost & Found: Recovery in Christ by Bruce Stanley
- Overcoming Emotional Obstacles through Faith: Navigating the Mind Field by Anthony Acampora, Director of Banyan’s Faith in Recovery Program
- The Case for Christ by Lee Strobel
Mental Health Resources for Recovery
Lumina Recovery consist of both mental health and substance abuse treatment facilities, meaning we offer mental health resources as well as chemical dependency resources. What’s more, addiction often co-occurs with mental illness, making these resources ever more important.
Below are some resources for mental health recovery that can help you or your loved one:
- This Emotional Life video series
- No Kidding, Me 2!! with Joe Pantoliano
- Dare: The New Way to End Anxiety and Stop Panic Attacks by Barry McDonagh
- Pleasure Unwoven: An Explanation of the Brain Disease of Addiction by Kevin McCauley
- Declutter Your Mind: How to Stop Worrying, Relieve Anxiety, and Eliminate Negative Thinking by S.J. Scott and Barrie Davenport
Call Us Today – (877) 716-7515

