
Our Addiction Resources
Navigating the world of addiction and recovery can be overwhelming. We’re here to provide clear, compassionate education and guidance. From practical advice for maintaining sobriety to informational guidance on the long-term effects of substance abuse, our content is a beacon of hope and understanding.
Our Team is Ready are ready to take your call
Call us Today!
or we can call you. Fill out form below
Our Blog

What Is Coke Jaw?
Coke jaw is a term that refers to excessive jaw clenching, grinding, and involuntary jaw movement caused by cocaine abuse. This condition can lead to jaw pain, dental problems, and temporomandibular joint (TMJ) disorders, significantly affecting a person’s quality of life.
Cocaine is a powerful stimulant drug that affects the central nervous system, leading to increased energy, heightened alertness, and muscle hyperactivity. One of the most common side effects of cocaine is involuntary muscle contractions, particularly in the jaw muscles, resulting in what is commonly known as cocaine jaw or coke jaw.
Understanding the symptoms of coke jaw, its causes, and available treatment options is essential for those struggling with substance abuse and its physical consequences.
How Cocaine Affects Your Mouth
Cocaine is highly addictive and affects dopamine levels in the brain, which play a role in muscle control.1 This overstimulation causes jaw muscles to tighten, often resulting in:
- Persistent jaw clenching
- Teeth grinding (bruxism)
- Facial muscle spasms
- Difficulty relaxing the jaw
Because cocaine also has a numbing effect, individuals may not notice the extent of jaw pain, dental damage, or muscle strain until the condition becomes severe.
Causes of Coke Jaw
The primary cause of coke jaw is cocaine’s impact on the central nervous system. As a powerful stimulant drug, cocaine increases dopamine release, which overstimulates muscle activity, leading to involuntary jaw movement.1 Other contributing factors include:
- Muscle hyperactivity – Cocaine disrupts normal muscle control, causing excessive tension in the jaw muscles.
- Bruxism (grinding teeth) – Increased dopamine activity leads to repetitive teeth grinding.
- Altered pain perception – Cocaine’s numbing effects prevent users from recognizing jaw pain and dental damage.
- Stress and anxiety – Cocaine use often heightens stress and anxiety, further increasing jaw clenching.
Over time, the combination of these effects leads to severe dental problems and chronic jaw pain.
Symptoms of Coke Jaw
Recognizing the symptoms of cocaine jaw early is essential for preventing long-term damage.
In the initial stages, individuals may experience mild jaw pain and stiffness, often accompanied by occasional teeth grinding. During and after cocaine use, users may notice an increase in jaw movement, excessive clenching, and tension in the jaw muscles. Some also report heightened tooth sensitivity, as the constant grinding begins to wear down the enamel.2
As the condition progresses, the signs of cocaine jaw become more severe. Individuals may develop persistent jaw pain and chronic muscle tightness, making it difficult to relax their jaw. Teeth grinding can intensify, leading to cracked or fractured teeth and significant dental erosion.2
The gums may start to recede, increasing the risk of gum disease (gingivitis) and potential tooth loss.2 Some users also experience TMJ disorders, which can cause difficulty opening and closing the mouth, as well as persistent facial pain and headaches.
Long-Term Consequences of Coke Jaw
Over time, the excessive strain on jaw muscles and teeth can lead to lasting structural damage. Severe enamel erosion and fractures increase the likelihood of tooth loss, while restricted blood flow to the gums heightens the risk of infections and periodontal disease.2
Chronic jaw clenching can also contribute to TMJ disorders, causing persistent facial and neck pain that interferes with daily life.
The Effect of Cocaine Abuse on Oral Health
Cocaine use has several dental-related side effects that can cause long-term damage. The effects of cocaine abuse on oral health include:2
- Cluster headaches
- Teeth grinding (bruxism)
- Palate and nasal cavity deterioration
- Rhinitis and chronic sinusitis
Over time, this repeated strain on the jaw muscles leads to jaw pain, TMJ disorders, and even tooth loss.
Differentiating Coke Jaw From Other Conditions
Coke jaw can sometimes be mistaken for other conditions, such as TMJ and bruxism.
TMJ disorders can be caused by genetics, arthritis, or injury, but coke jaw is directly linked to cocaine use. Some individuals grind their teeth due to stress or sleep disorders, while coke jaw results from drug-induced muscle hyperactivity.
The key difference is that coke jaw symptoms typically occur during and after cocaine use and worsen with continued substance abuse.

Treatment Options for Coke Jaw
Early intervention is key to preventing long-term damage. If you’re experiencing coke jaw, taking the following precautions can help reduce damage:
- Use a mouthguard to protect your teeth from grinding.
- Apply warm compresses to relax jaw muscles.
- Avoid hard foods to reduce strain on the jaw.
- Stay hydrated to improve saliva production and prevent dry mouth.
Professional Dental Care
Seeking professional dental care is essential for managing the side effects of cocaine use on oral health. Treatment options may include:
- Dental crowns, veneers, and fillings to repair cracked or worn-down teeth.
- Braces or bite guards to correct alignment issues caused by excessive jaw clenching.
- Specialized treatments to relieve jaw pain and improve jaw movement.
Addressing Addiction Through Treatment Programs
Because coke jaw is directly linked to cocaine use, overcoming substance abuse is essential for long-term recovery and preventing further oral health complications. Treatment programs for cocaine addiction include:
- Supervised withdrawal management helps individuals safely stop using cocaine while addressing withdrawal symptoms.
- Cognitive behavioral therapy (CBT) helps individuals recognize and change harmful thought patterns related to drug use.
- Inpatient and outpatient rehab provides medical and psychological support to overcome addiction.
Seeking help for substance abuse can not only improve overall health but also prevent further dental problems caused by coke jaw.
Preventing Coke Jaw and Protecting Your Health
The best way to prevent coke jaw is to avoid stimulant drug use, as eliminating the root cause can stop the involuntary jaw movement and teeth grinding associated with cocaine use. Managing stress is also important, as heightened anxiety can contribute to jaw clenching and muscle tension.
Find Help for Cocaine Abuse With Lumina Recovery
If you or someone you care about is facing cocaine addiction and noticing signs of coke jaw, support is within reach.
Lumina Recovery offers comprehensive treatment programs, including detox services and cognitive behavioral therapy (CBT), to help individuals safely stop using cocaine and heal from its effects.
Call Lumina Recovery today and take the first step toward a healthier future.
Sources:
- National Institute on Drug Abuse. Cocaine.
- Healthline. How Cocaine Impacts Your Teeth and Mouth.

Can You Get Addicted to Benadryl?
Yes, while Benadryl is not considered highly addictive in the traditional sense, misuse of the drug can lead to dependence and withdrawal symptoms.
Benadryl, the brand name for diphenhydramine, is a common over-the-counter medication used to treat symptoms of allergies and allergic reactions such as watery eyes and nasal congestion. It also acts as a sleep aid due to its sedative effect.
While Benadryl is generally safe when used as directed, concerns about its misuse and potential for addiction have been growing.
What Is Benadryl?
Benadryl is an antihistamine that works by blocking histamine receptors in the brain and body.1 It is commonly used to relieve symptoms of allergic reactions, the common cold, and motion sickness. Due to its sedative effect, it is also an ingredient in many sleep aid medications.
It is available in various forms, including tablets, capsules, and liquid solutions, and is widely used for both short-term relief and symptom management. Recommended doses vary based on age and condition, and it is important to follow proper dosage instructions to ensure safe and effective use.
Benadryl Addiction Potential
Addiction is characterized by compulsive drug use despite negative consequences, whereas dependence refers to the body’s reliance on a substance. While Benadryl is not classified as an addictive drug in the same way as opioids or stimulants, it is possible to develop a psychological dependence, particularly for relieving symptoms like insomnia or anxiety.
Benadryl does not cause the same chemical dependence as opioids or stimulants.1 However, frequent use, especially beyond recommended doses, can lead to both short-term and long-term reliance on the drug to induce sleep or reduce anxiety.
Potential for Misuse and Dependence
Some individuals misuse Benadryl for its sedative effects or, in high doses, for its euphoric effects. These higher doses can create temporary hallucinations, heightened drowsiness, and cognitive impairment.
People with sleep disorders or anxiety may unknowingly develop a dependence on Benadryl, using it as a sleep aid instead of seeking safer medical alternatives.
As tolerance increases, individuals may take larger doses of Benadryl to achieve the same sedative effect, increasing their risk of experiencing side effects of Benadryl such as blurred vision, dizziness, and low blood pressure. Prolonged misuse can lead to difficulty sleeping without the drug, further reinforcing the cycle of dependence.2
Because Benadryl is readily available, many individuals mistakenly believe it carries little risk, leading to frequent misuse. However, habitual overuse may contribute to severe health concerns such as memory problems, confusion, and even increased risks of dementia with prolonged use.2
One alarming trend associated with Benadryl misuse is the “Benadryl Challenge,” a viral social media trend on TikTok that encourages individuals, particularly teenagers, to take dangerously high doses of the drug to experience hallucinations.
This challenge has resulted in hospitalizations and, in some cases, fatalities, prompting the FDA and medical professionals to issue strong warnings against participating in or promoting such behavior.1
Individuals who take Benadryl frequently may also experience withdrawal symptoms that reinforce continued use, making it even harder to stop without proper medical guidance.
Signs and Symptoms of Benadryl Addiction
Recognizing the signs of Benadryl addiction is essential for early intervention. The symptoms of addiction can be physical and behavioral, making it important to identify changes in usage patterns before they become severe.
Physical Symptoms
- Increased tolerance requiring higher doses of Benadryl
- Withdrawal symptoms such as headaches, nausea, and insomnia
- Persistent drowsiness or blurred vision
- Heart palpitations or increased heart rate
Behavioral Signs
- Using Benadryl compulsively or in ways not recommended
- Neglecting responsibilities at work, school, or home
- Social withdrawal or secretive behavior
- Experiencing cravings for Benadryl
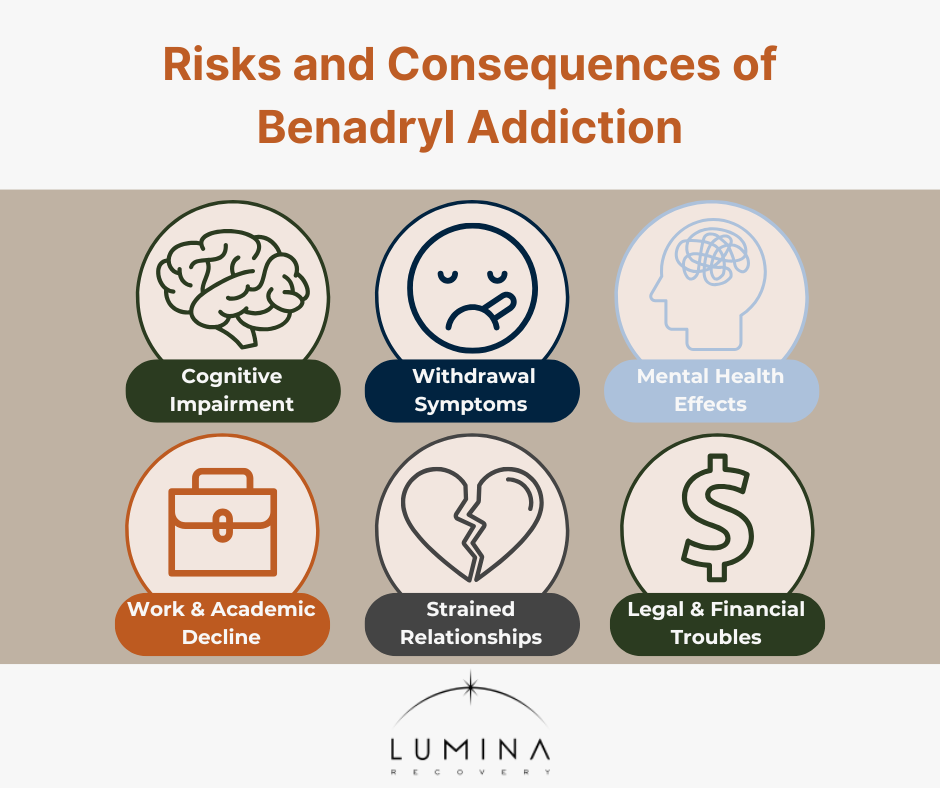
Risks and Consequences of Benadryl Addiction
Long-term Benadryl misuse can have serious health and lifestyle consequences. From cognitive decline to cardiovascular risks, excessive use of this easily accessible medication can lead to both immediate and long-term harm.2
Long-Term Health Risks
- Cognitive Impairment: Long-term Benadryl use has been linked to memory problems and an increased risk of dementia.
- Withdrawal Symptoms: Excessive use may result in withdrawal effects such as insomnia, sweating, and nausea.
- Mental Health Effects: Anxiety, depression, and psychosis can develop from chronic misuse.
Impact on Daily Life
- Work and Academic Decline: Drowsiness and impaired cognition can affect performance.
- Strained Relationships: Misuse may cause conflicts with family and friends.
- Legal and Financial Troubles: If excessive use leads to accidents or medical emergencies, there may be financial consequences.
Benadryl Withdrawal
When a person stops using Benadryl after prolonged misuse, they may experience withdrawal symptoms. The intensity and duration of withdrawal depend on dosage, frequency of use, and individual health factors.
Common withdrawal symptoms of Benadryl can include insomnia or difficulty sleeping, increased heart rate, excessive sweating, increased saliva production, and enlarged pupils.3 These symptoms can vary in intensity depending on the level of dependence and frequency of use.
Mild cases may resolve within a few days, while severe dependence may require medical support.

Treatment Options for Benadryl Addiction
Recovering from Benadryl addiction requires a combination of professional medical advice and therapeutic interventions.
Medical Interventions
A supervised detox program can help individuals taper off Benadryl safely while managing withdrawal symptoms. In cases of persistent sleep or anxiety issues, medications may be recommended to ease withdrawal symptoms or manage underlying conditions.
Therapeutic Approaches
Cognitive behavioral therapy (CBT) helps individuals identify triggers and develop healthier coping strategies. Support groups such as Narcotics Anonymous (NA) or other peer support networks provide community-based encouragement.
Individual counseling with a therapist can address underlying causes of dependence, such as anxiety or insomnia.
Holistic and Lifestyle Approaches
Incorporating holistic strategies can support long-term recovery. Practices such as mindfulness meditation, yoga, and exercise can help manage anxiety and improve sleep quality without reliance on medication.
Establishing a consistent sleep routine, reducing caffeine intake, and engaging in relaxation techniques can also help manage withdrawal symptoms and improve sleep quality.
Frequently Asked Questions (FAQ)
Is it okay to take Benadryl every night?
While taking Benadryl occasionally for sleep is common, frequent use can lead to psychological dependence and increase the risk of long-term health issues, including memory problems.
Can you get Benadryl withdrawal?
Yes. People who use Benadryl regularly and suddenly stop may experience withdrawal symptoms like insomnia, increased saliva production, increased heart rate, excessive sweating, and enlarged pupils.3
What happens if you use Benadryl every day?
Daily use can result in increased tolerance, psychological dependence, and cognitive impairment. Short-term and long-term use have also been associated with an increased risk of dementia and other health complications.
Get the Support You Deserve With Lumina Recovery
Seeking professional treatment is the best way to overcome Benadryl dependence. Specialized programs provide comprehensive care for short-term and long-term solutions.
Lumina Recovery provides detox programs to manage withdrawal safely and cognitive behavioral therapy (CBT) to address the underlying causes of addiction. Our personalized treatment plans support lasting recovery and overall well-being.
Don’t let Benadryl dependence control your life. Contact Lumina Recovery today for a confidential consultation and take the first step toward healing.
Sources:
- FDA. FDA warns about serious problems with high doses of the allergy medicine diphenhydramine (Benadryl).
- Healthline. Benadryl Side Effects: Examples and Treatment Options.
- Saran JS, Barbano RL, Schult R, Wiegand TJ, Selioutski O. Chronic diphenhydramine abuse and withdrawal: A diagnostic challenge. Neurol Clin Pract. 2017 Oct;7(5):439-441. doi: 10.1212/CPJ.0000000000000304.

Is Naproxen Addictive? Everything You Need to Know
No, naproxen is not classified as an addictive drug, but it can still be misused, and long-term use may lead to dependence in some individuals. It is a common over-the-counter medication and prescription nonsteroidal anti-inflammatory drug (NSAID) used to reduce pain and inflammation.
However, many people wonder if prescribed naproxen carries the risk of addiction like some other pain relievers. Knowing how naproxen works, its potential for misuse, and the side effects of naproxen can help individuals make informed decisions.
What Is Naproxen?
Naproxen is a widely used nonsteroidal anti-inflammatory drug (NSAID) that helps manage pain, inflammation, and fever. Unlike opioid painkillers, it does not interact with the brain’s opioid receptors or produce euphoric effects.
There are two types of prescription naproxen:
- Naproxen
- Naproxen sodium
Both forms are considered equally safe and effective. However, naproxen sodium is often absorbed more quickly, making it a preferred choice for individuals who need faster pain relief.1
Prescription naproxen is sold under the brand names Anaprox DS, Naprelan, and Naprosyn. Naproxen sodium, like Aleve, is also available over the counter.
Due to its effectiveness in treating pain, it is commonly prescribed for various conditions including:1
- Rheumatoid arthritis
- Osteoarthritis
- Ankylosing spondylitis
- Menstrual cramps
- Bursitis
- Tendinitis
- Acute gout
After taking a dose, naproxen’s effects last up to 12 hours, and traces of the drug can be detected for up to four days. Depending on the condition being treated, individuals may take naproxen every 6 to 12 hours and typically use it only until symptoms subside.1
Is Naproxen Considered a Narcotic?
A narcotic is a drug that affects the central nervous system, producing pain relief and, in some cases, euphoria, which can lead to addiction. Opioids such as oxycodone and morphine fall into this category.
Naproxen, however, is not classified as a narcotic. Because it does not interact with opioid receptors, it does not produce the same euphoric effects that contribute to opioid addiction.
Unlike opioids, which are commonly used for both acute and chronic pain, naproxen does not carry the same risk of misuse or addiction.1 Opioids, while effective for severe pain, are highly potent and often lead to dependence.
For those needing sustained pain relief, naproxen is a safer alternative when used correctly under the guidance of a healthcare provider.
Assessing the Addictive Potential of Naproxen
When evaluating naproxen’s potential for addiction, it is important to understand how it interacts with the body. Unlike substances that influence the brain’s reward system, naproxen primarily works by reducing inflammation and blocking pain signals at the source.2
Addiction is often associated with compulsive use, cravings, and withdrawal symptoms, but naproxen typically does not exhibit these characteristics. Its mechanism of action does not alter brain chemistry in a way that leads to psychological or physical dependence. Instead, it provides relief from pain by inhibiting enzymes responsible for inflammation.2
Long-term use of any medication should be monitored by a healthcare professional to ensure it is being taken appropriately. When individuals rely on naproxen for ongoing pain management, this reliance is not classified as addiction. It is essential to follow dosing recommendations to maximize its benefits and ensure effective pain relief.
For those managing chronic pain, naproxen serves as a widely trusted option that provides relief without affecting the brain’s dependency pathways. Understanding its role in pain management allows individuals to use it safely and effectively under medical guidance.
Potential Risks and Side Effects of Naproxen
Although naproxen is not addictive, it does have short-term side effects.1 However, misuse, prolonged use, or taking larger doses can lead to serious long-term health risks.3
Short-Term Side Effects
- Nausea and vomiting: Common temporary effects, especially when taken on an empty stomach.
- Heartburn or indigestion: Can occur due to irritation of the stomach lining.
- Dizziness: May cause lightheadedness in some individuals.
Long-Term Risks
- Gastrointestinal damage: Increased risk of ulcers, stomach bleeding, and irritation.
- Cardiovascular risks: Higher doses over a long time may increase the risk of high blood pressure, heart attacks, and strokes.
- Kidney damage: High doses or extended use can lead to kidney function decline.

Recognizing and Addressing Misuse
Although naproxen is not considered addictive, some individuals may misuse it, particularly for chronic pain. Signs of misuse include:
- Taking high doses beyond recommended limits
- Using naproxen for reasons other than pain relief
- Relying on naproxen frequently despite negative health effects
- Ignoring medical advice about dosage restrictions
- Taking naproxen alongside nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, increasing risks
- Drinking alcohol while on naproxen, worsening gastrointestinal side effects
- Experiencing persistent high blood pressure due to naproxen overuse
If you or a loved one is misusing naproxen, consider the following steps:
- Ask medical professionals for guidance on safer pain and inflammation management alternatives.
- Explore non-medication pain relief methods such as physical therapy or lifestyle changes.
- Seek addiction treatment and counseling for chronic pain management strategies.
- Follow safe dosing recommendations, such as taking the prescribed naproxen only under the supervision of a doctor.
- Always take naproxen with food or milk to reduce stomach irritation and avoid long-term complications.
- Consult your doctor for rheumatoid arthritis or chronic conditions that require extended naproxen use.
FAQs
Can you develop a tolerance to naproxen?
Unlike opioids, naproxen does not lead to tolerance in the same way. However, long-term users may find that their pain returns if the underlying condition worsens, leading them to increase their dose.
Is it safe to combine naproxen with other pain relievers?
It depends on the type of pain reliever. Avoid taking naproxen with other nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or aspirin, as this increases the risk of stomach ulcers and bleeding. However, naproxen can be combined with acetaminophen (Tylenol) for pain relief under medical supervision.
What should you do if you forget a dose?
If you miss a dose, take it as soon as you remember. However, if your next dose is within a few hours, skip the missed dose—do not double up to compensate.
Find Supportive Treatment With Lumina Recovery
Naproxen is not addictive like opioids, but improper use can still lead to health risks. While it does not cause dependency, excessive or prolonged use may result in gastrointestinal, cardiovascular, or kidney damage.
At Lumina Recovery, dual diagnosis treatment can help address underlying mental health conditions that may contribute to medication reliance. Additionally, cognitive behavioral therapy (CBT) provides effective strategies for managing pain and inflammation without overuse of medication.
If you or a loved one needs guidance on safer pain relief management and addiction treatment options, contact Lumina Recovery today for expert support.
Sources:
- Healthline. Naproxen, Oral Tablet.
- WebMD. Pain Relief: How NSAIDs Work.
- NHS. Common questions about naproxen.

How to Find Joy in a Sober Lifestyle
Many believe that giving up alcohol or drugs means losing fun and excitement. In active addiction, we trap ourselves in the illusion that chemical euphoria equals happiness. This false joy is fleeting—always requiring more substances just to feel normal, while the inevitable crash leaves us worse off than before.
The cycle is relentless: use, crash, isolate, and damage relationships, only to use again to numb the pain. True joy becomes a distant memory in addiction’s grip. Yet, amidst this struggle, there is hope. Sobriety opens the door to authentic happiness and meaningful experiences that no substance can replicate.
Below, we’ll explore five areas you can tap into for finding joy in sobriety and living a more fulfilling life.
1: Redefining Joy in Recovery
True happiness in sobriety comes from shifting your perspective and embracing personal growth. By setting realistic expectations and celebrating small wins, you create a foundation for lasting fulfillment.
Shifting Perspectives
Setting realistic expectations in early recovery is crucial to preventing relapse. While substance use floods the brain with dopamine, quitting leads to a temporary decrease, which can result in numbness or depression. But rest assured, this phase is temporary.
With exercise, nutrition, and abstinence, your brain will rebalance. You may feel disheartened at first, but hold on—genuine joy awaits you in meaningful experiences that far surpass fleeting highs.
Understanding Fulfillment
Personal growth begins with small steps. Each achievement builds purpose and self-worth. As your confidence grows, you’ll confront your past and acknowledge your value. This healing process brings inner peace, eliminating the need for substances.
Celebrating Small Wins
Begin a gratitude list by noting daily blessings, such as the support of sober friends or the comfort of a warm bed. Recognize your progress—like staying sober today and receiving positive feedback from your counselor on your newfound radiance and improving health. These moments are truly precious.
2: Reconnecting With Passions and Interests
Sobriety gives you the freedom to explore new passions and rediscover activities that bring you genuine joy. Engaging in hobbies, creativity, and physical pursuits can help fill your life with excitement and purpose.
Exploring New Hobbies
Delve into hobbies that capture your full concentration or allow for physical engagement—activities that you love enough to savor without the dulling effects of substances. Consider martial arts, mountain biking, or spirited debates.
Pursuing Creative Endeavors
The avenues for artistic and creative self-expression are virtually limitless. Platforms like Pinterest and YouTube offer rich sources of inspiration. Consider experimenting with cooking, taking singing lessons, or writing an e-book.
You might also discover joy in simpler pleasures, like a walk in the park or striking up a conversation with a stranger. The more deeply you engage in these activities, the more meaningful they become, bringing you happiness in sobriety.
Incorporating Physical Activities
Exercise, sports, and outdoor adventures all require a clear head—ideal for finding joy in sobriety. Relish the natural high from hiking in the mountains or doing yoga on the beach. Extreme sports like scuba diving, zip-lining, or parasailing can get the adrenaline pumping. Or start small—even a simple bike ride can bring fulfillment.
3: Building Meaningful Relationships
One of the most rewarding aspects of sobriety is building deeper, more authentic connections. Strengthening bonds, making new friends, and fostering trust can lead to a more fulfilling social life.
Strengthening Bonds
Relearning how to connect with family and friends without drugs or alcohol takes time. Begin by showing love and understanding. Be present both emotionally and physically—like cooking a meal for your family or taking a friend’s child to the park. These actions deepen connections as loved ones witness your growth and gradually begin to trust you again.
Making New Connections
People often use substances to ease social anxiety, but this often fails because, after a certain point, one can become too drunk or stoned to hold a conversation. Break this cycle by joining sober communities, interest groups, or support networks where you can form authentic relationships without the pressure of drinking. Your chances of meeting genuine friends will be exponentially higher!
Fostering Authenticity
Build relationships based on mutual respect, trust, and shared values. Avoid falling back into old drinking circles. Connect with people who understand your journey and will encourage you in all you aspire to become.

4: Practicing Self-Care and Mindfulness
Taking care of your mental, physical, and emotional well-being is essential in recovery. Prioritizing self-care and staying present in the moment can help you build a balanced, joyful life.
Prioritizing Mental Health
Incorporate therapy, meditation, or journaling to maintain emotional balance. Mindfulness can help reduce the shame associated with addiction, revealing that true happiness was seldom present during those years. Sobriety allows you to address unresolved mental health issues—issues that may have contributed to your substance use—so you can move forward in wellness.
Focusing on Physical Well-Being
Your body may be recovering from malnourishment. Collaborate with a nutritionist to create a diet that supports your physical and mental health. As you navigate sobriety, you might crave sugar—a nutritionist can help you manage these cravings.
Living in the Moment
Engage fully with experiences as they unfold instead of being preoccupied with the past or future. By focusing on the present, we become attuned to our feelings and surroundings, allowing us to thrive in everyday moments.
5: Finding Purpose and Giving Back
A meaningful life in sobriety often comes from discovering your purpose and helping others. Volunteering, achieving personal goals, and celebrating progress can provide a deep sense of fulfillment.
Discovering Purpose
In sobriety, long-held dreams become attainable. Whether it’s returning to school, joining a boxing club, or staying informed through the news, countless opportunities await. Focus on honing your social skills and cultivating genuine curiosity in conversations, helping you present your best self to others.
Volunteering
Discover the joy of giving back to the community. Spend a few hours each week reading to the elderly, volunteering at a dog rescue center, or organizing food distribution for the homeless. Supporting individuals in recovery at local detox centers can forge deep connections that enrich both your life and theirs.
Celebrating Achievements
As you emerge from the fog of addiction, you begin anew with honesty, choosing a life truly worth living. It takes immense courage to take charge of your destiny. Reflect on your growth and milestones—these are your sources of pride and motivation.
Escaping the cycle of alcohol or drugs is a significant achievement. As you learn to love and trust yourself again, you’ll discover that a wonderful life awaits you.
Lumina Recovery: Embrace Joy and Thrive in Sobriety!
Are you ready to transform your life and find genuine joy in recovery? We understand the complexities of your journey and have witnessed countless transformations that demonstrate how rewarding sobriety can be.
Our dedicated team creates a nurturing environment with a holistic approach to treatment, integrating therapy, community support, and holistic practices to guide you through addiction while reigniting your passions and purpose.
Take the first step with Lumina Recovery—your new, vibrant life awaits!

The Power of Addiction Recovery Support Groups
Support groups play a vital role in addiction recovery, offering a sanctuary for those in need. They create an environment where individuals can find solace and build relationships—especially during times when friends and family may be distant.
Beyond providing emotional support, these groups serve as a source of accountability, encouragement, and practical guidance, helping individuals stay committed to their sobriety.
Below, we’ll explore what support groups are, the different types available, and the profound benefits they offer. We’ll also share practical tips on how to get the most out of these groups, ensuring that individuals can fully embrace the power of community in their recovery journey.
What Are Support Groups for Addiction Recovery?
Support groups unite individuals facing similar challenges, creating a welcoming space for everyone. These gatherings bring together people from diverse backgrounds, deepening mutual understanding and encouraging support among members. Whether led by peers or professionals, each group emphasizes a safe space for open conversation.
By sharing personal stories and coping strategies, members gain valuable insights, broaden their perspectives on recovery, and strengthen their commitment to their individual journeys.
Types of support groups for addiction recovery:
- 12-step programs (e.g., AA, NA)
- Non-12-step alternatives (e.g., SMART Recovery, Refuge Recovery)
- Faith-based and secular options
- Specialized groups for specific demographics (e.g., LGBTQ+, veterans, women-only)
The significance of shared understanding within these groups cannot be overstated. They provide a non-judgmental atmosphere, allowing individuals to express their struggles candidly without the fear of stigma or criticism—a crucial aspect for effective healing and connection.
The Benefits of Support Groups
These groups not only address the immediate issues of addiction but also empower individuals to develop long-term strategies for sustaining sobriety.
Connection and Belonging
Isolation is often a hallmark of addiction, and support groups work diligently to dismantle that barrier. By engaging with others who understand these struggles, individuals can form bonds that enhance their sense of community. This connection not only offers comfort but can significantly bolster motivation and resilience throughout the recovery journey.
Accountability
Support groups provide a critical framework for accountability. Members share their goals and progress during meetings, cultivating a sense of responsibility both to themselves and to one another. This accountability helps individuals stay focused on their recovery objectives. Knowing that others are invested in their successes can inspire commitment, even in the face of setbacks.
Emotional Support
Confronting the complexities of recovery can be overwhelming, and emotional backing from these groups is invaluable. They provide a trusting atmosphere where individuals can voice their thoughts, fears, and frustrations. Sharing experiences often leads to receiving support and insights from peers who have faced similar adversities—reinforcing the notion that no one must confront recovery alone.
Learning Opportunities
Support groups offer a wealth of learning. Members can share effective strategies, coping techniques, and valuable lessons learned throughout their journeys. This collective knowledge empowers individuals to make informed decisions about their paths to recovery and to learn from both victories and obstacles faced within the group.
Inspiration and Hope
Witnessing the progress of others within support groups can be incredibly motivating. Hearing stories of resilience can reignite hope, reminding participants that change is achievable. Observing peers confront their own hardships serves as a powerful incentive, encouraging individuals to remain dedicated to their well-being.

How to Get the Most Out of Support Groups
To fully benefit from support groups for addiction recovery, active engagement is essential.
1: Be ready to commit.
Consistency is vital. By attending regularly, individuals not only demonstrate their dedication to recovery but also strengthen the group dynamic. A reliable presence builds trust and deepens relationships, essential components of a supportive community. Regular attendance cultivates familiarity, enabling participants to track each other’s progress and celebrate milestones together.
2: Go in with an open mind.
Enter each group meeting with a receptive heart and mind. Every participant contributes unique insights that can enhance the experience for all. Being willing to listen as much as to share invites a dynamic exchange of ideas and experiences, paving the way for profound personal growth.
3: Allow yourself to be vulnerable.
Authenticity lays the groundwork for true connections. Sharing struggles openly fosters deeper bonds and enriches the exchange of support. Though it can be daunting, vulnerability often catalyzes meaningful relationships and provides the encouragement needed to thrive.
4: Practice respect.
The foundation of a respectful atmosphere rests on mutual regard. Participants should honor one another’s experiences, recognizing that each road traveled is uniquely personal. Establishing boundaries and maintaining a judgment-free space cultivates a flourishing community.
5: Find the right fit.
Discovering the ideal support group may require some exploration. Engaging with various groups allows individuals to pinpoint one that resonates with their personal values and aspirations. The right fit can significantly impact their healing journey.
6: Seek balance.
While support groups for addiction recovery are invaluable, they should complement other transformative strategies, such as professional therapy, tailored recovery plans, and self-care practices. Embracing a holistic approach encourages a deeper and more integrated healing experience.
Step Into Transformation: Discover Your Community at Lumina Recovery!
If you or someone you care about struggles with addiction, consider a life-changing opportunity within a community that truly understands. At Lumina Recovery, we embrace a holistic approach to healing that prioritizes not just recovery but connection, empowerment, and the celebration of each individual’s journey.
Our diverse treatment options address a broad range of needs, ensuring you find a welcoming space to be your authentic self. Here, you are not just another face in the crowd—you are part of a family dedicated to your growth and well-being.
Take a bold step into your future—your path to renewal awaits. Experience the warmth of belonging and the power of shared stories that inspire hope.
Together, let’s build a foundation for lasting recovery and rediscover the vibrant joy of living a fulfilled life.

8 Tips for a Sober St. Patrick’s Day
St. Patrick’s Day, celebrated every March 17th, honors Ireland’s patron saint and has evolved into a global celebration of Irish culture. While parades and green attire are common, the day has also become closely tied to drinking traditions.
For those in recovery, this association can make the holiday challenging. However, celebrating without alcohol opens the door to meaningful connections, improved health, and clear memories.
Celebrating a sober St. Patrick’s Day doesn’t mean missing out on fun. Instead, it creates opportunities to focus on culture, tradition, and quality time with friends and family. With careful planning and creative activities, you can make this St. Paddy’s Day enjoyable and meaningful while staying alcohol-free.
1. Plan Ahead to Stay Focused and Sober
Preparation is key to maintaining sobriety during celebrations. Start by identifying potential triggers, such as parties where alcohol is served, and develop strategies to avoid or handle them.
Let your friends and family know about your sobriety goals to set expectations and gain support. It’s also wise to arrange transportation or have an exit plan if you feel uncomfortable. Knowing your game plan reduces stress and keeps you focused on your priorities.
Having a sober friend with you can provide extra encouragement and accountability. You might also consider attending a support group meeting before or after your celebrations to reinforce your commitment to sobriety.
2. Host a Sober Celebration at Home
Hosting your own St. Patrick’s Day gathering puts you in control of the environment. Decorate with Irish-themed accents such as shamrocks, green tableware, and other festive items to set the mood. Plan engaging activities like board games, karaoke, or a movie marathon featuring Irish films.
Provide non-alcoholic drink options, such as sparkling waters, sodas, or homemade mocktails. For example, mix lime juice, ginger beer, and a splash of mint syrup for a refreshing St. Patrick’s Day twist.
Pair your drinks with a traditional Irish meal like Irish stew or shepherd’s pie. Cooking together with friends and family can be a fun and rewarding way to bond. Incorporating traditional Irish dishes and desserts ensures your sober St. Patrick’s Day celebration feels festive and complete.
3. Explore Alcohol-Free Events in Your Area
Many cities host St. Patrick’s Day parades, cultural festivals, and community fairs that are family-friendly and alcohol-free. Check local event listings for St. Patrick’s Day concerts, Irish-themed art shows, or outdoor activities.
Some areas even have sober meetups or support group events focused on celebrating holidays without alcohol. If local options are limited, consider virtual events where you can connect with others celebrating sober.
Look for alcohol-free activities and events featuring Irish music, dance performances, or craft fairs. Attending these events can deepen your appreciation for Irish culture while allowing you to celebrate in a safe, supportive environment.
4. Dive into Irish Culture and Traditions
Celebrate St. Patrick’s Day by immersing yourself in Irish culture. Try cooking traditional Irish dishes like shepherd’s pie, colcannon, or soda bread. Don’t forget to include Irish stew, a hearty and satisfying meal perfect for the occasion.
Learn Irish dance steps through online tutorials or enjoy Irish folk music playlists. Use the holiday as an opportunity to explore Irish history, folklore, and symbols. Activities like these provide engaging conversation starters and deepen your appreciation for Irish culture.
Incorporate storytelling by sharing Irish legends or myths with your friends and family. This activity adds a fun, educational twist to your alcohol-free celebration.

5. Prioritize Self-Care and Reflection
St. Patrick’s Day can also be a time for gratitude and reflection. Use the day to celebrate your sobriety journey. Meditate, journal about your progress, or make a list of things you’re thankful for. If you need extra support, reach out to your sober community or attend a support group meeting. Prioritizing self-care reinforces your commitment to sobriety and boosts confidence.
Taking time for yourself can make your sober St. Patrick’s Day even more meaningful. Consider setting goals for the year ahead or writing letters to loved ones to express gratitude for their support.
6. Fun Activities to Replace Drinking Traditions
Replace drinking traditions with creative activities that keep you engaged and entertained. Organize a scavenger hunt with Irish-themed clues or enjoy the outdoors with a hike to appreciate the fresh air.
Craft projects, like making shamrock decorations or painting Irish landscapes, can be fun and relaxing. Host a trivia night focused on Irish history and culture to keep the celebration lively.
Invite friends and family to participate in these activities to make the day interactive and memorable. You can also include fun games like charades or Irish-themed bingo.
7. Non-Alcoholic Drink Ideas for the Holiday
Festive beverages don’t have to include alcohol. Try these non-alcoholic drink ideas to keep the celebration fun:
Shamrock Punch: Blend lime sherbet with lemon-lime soda and garnish with mint leaves.
Sparkling Apple Spritz: Mix sparkling water with apple juice and a splash of lime.
Green Tea Cooler: Brew green tea, chill it, and add honey, lemon, and fresh mint.
You can also explore zero-proof beverage brands for ready-made options or mocktail recipes to impress your guests.
8. Connect With Like-Minded Communities
Being part of a sober community can help you feel supported and inspired. Join online forums, read sobriety-focused blogs, or visit websites to share experiences and ideas.
Participate in hashtags like #SoberStPatricksDay to connect with others celebrating sobriety. Whether in person or online, engaging with like-minded people strengthens your commitment to sobriety.
Attending a support group event can also provide comfort and encouragement, especially if you’re celebrating sober for the first time.
Celebrate Sober and Thriving With Lumina Recovery
St. Patrick’s Day is a chance to embrace culture, connection, and fun without alcohol. At Lumina Recovery, we offer outpatient programs and dual diagnosis treatment for those navigating recovery. These services provide the structure and support needed to maintain sobriety and focus on personal growth.
If you’re ready to celebrate life free from addiction, contact Lumina Recovery today to start your journey.

The Interconnected Relationship Between Gut Health and Addiction
Addiction is a complex condition that affects both the body and mind. It involves intricate interactions between genetics, environment, and neurobiology.
While traditional addiction treatments often focus on the brain and behavior, recent studies show a surprising possible contributor to addiction—gut health.1
The gut-brain axis, which connects the gut and brain through biochemical signaling, has emerged as a critical factor in mental health and behavior. Understanding this connection can provide new insights into addiction and recovery.
What Is the Gut-Brain Axis?
The gut-brain axis is a communication network linking the gastrointestinal tract and the central nervous system. This bidirectional connection relies on nerves, hormones, and immune signals to regulate mood, stress responses, and cravings. The vagus nerve plays an important role in this communication, transmitting signals between the gut and brain to influence behavior and brain function.2
Central to this axis is the gut microbiome, a collection of trillions of microorganisms residing in the digestive system. These microbes influence neurotransmitter production, such as serotonin and dopamine, which regulate mood and reward systems. A healthy gut microbiome supports emotional stability, while an imbalance—known as dysbiosis—may contribute to mental health disorders including anxiety, depression, and stress.3
Gut microbiome composition can directly affect the progression and persistence of substance use disorders. For example, disruptions in microbial diversity can impact the brain’s prefrontal cortex, which is responsible for decision-making and impulse control. Pro-inflammatory markers resulting from gut imbalances can impair brain function, further complicating addiction recovery.1
How Gut Health Influences Addiction
Understanding how gut health influences addiction provides valuable insight into the biological and psychological mechanisms that drive substance use disorders. The gut-brain axis plays a key role in regulating mood, cravings, and stress responses.
When this system is disrupted, it can increase susceptibility to addiction and hinder recovery efforts. Addressing gut imbalances may help improve mental health, stabilize cravings, and enhance overall recovery outcomes by restoring balance to both the body and mind.
1. Dysbiosis and Neurotransmitter Production
Dysbiosis can disrupt serotonin and dopamine levels, which are critical for mood regulation and impulse control. Imbalances may lead to cravings and compulsive behaviors, exacerbating addiction.
2. Inflammation and the Brain’s Reward System
Chronic gut inflammation can impair the brain’s reward pathways. Pro-inflammatory markers alter neurotransmitter signaling, potentially increasing vulnerability to addiction and relapse.
3. Short-Chain Fatty Acids
Beneficial bacteria in the gut produce short-chain fatty acids, which help maintain gut barrier integrity and reduce inflammation. Reduced levels of these fatty acids can lead to increased intestinal permeability, contributing to stress and addiction.
4. Gut-Brain Communication Disruptions
Damage to gut microbiota can affect how the vagus nerve transmits signals, reducing control over cravings and emotional responses.
Impact of Various Substances on Gut Health
The substances individuals consume can significantly affect gut health, which in turn impacts addiction and recovery processes.
Alcohol
Alcohol damages the gut lining, leading to increased intestinal permeability (leaky gut). It disrupts the balance of beneficial bacteria, reducing microbial diversity.
These changes promote inflammation and stress, amplifying addiction and impacting the gut-brain axis. In cases of alcohol use disorder, prolonged exposure may further alter gut microbiota, leading to systemic inflammation and affecting brain function.
Opioids
Opioids can slow gut motility, leading to constipation and gut microbiome imbalances. They can also impair microbial diversity, further weakening gut-brain communication.
Fentanyl
Fentanyl may exacerbate gut dysfunction by inhibiting gut motility and altering gut microbiome composition. Its impact on gut health may intensify dependence by heightening cravings and withdrawal symptoms.
The Role of Diet in Recovery
A nutrient-rich diet is essential for restoring gut health and supporting addiction recovery. Specific dietary strategies include:
1. Fiber-Rich Foods
Whole grains, fruits, and vegetables promote the growth of beneficial bacteria. Legumes and beans provide additional fiber to enhance gut microbiome diversity.
2. Fermented Foods
Yogurt, kimchi, and kefir provide probiotics to balance the gut microbiome. Sauerkraut and miso offer additional sources of probiotics for gut health.
3. Probiotics and Prebiotics
Probiotics introduce beneficial bacteria, while prebiotics (fiber) feed them, enhancing gut health. Garlic, onions, and bananas are excellent prebiotic sources to support bacterial growth.
4. Hydration
Drinking adequate water daily supports digestion, nutrient absorption, and gut balance. Herbal teas like peppermint or ginger can soothe the digestive tract and reduce inflammation.
5. Anti-Inflammatory Foods
Foods rich in omega-3 fatty acids, such as salmon and flaxseeds, help reduce inflammation and support microbial diversity. Berries and leafy greens offer antioxidants to combat oxidative stress and promote gut health.

Innovative Therapies Targeting the Gut-Brain Axis
Emerging treatments highlight the gut’s role in addiction recovery:
Microbiome-Based Therapies
Probiotic and fecal microbiota transplants are being studied for their potential to restore gut balance and improve mental health. Prebiotic supplements are being explored to stimulate the growth of beneficial bacteria and enhance gut health.
Nutritional Psychiatry
Diet-focused treatments aim to alleviate addiction symptoms by enhancing gut health. Customized meal plans targeting gut health may provide personalized support for addiction recovery.
Gut Health Testing
Tests to evaluate microbial diversity and gut inflammation are becoming tools for personalized treatments. Stool analysis tests are gaining popularity to provide insights into gut microbiome imbalances and guide treatment approaches.
5 Practical Steps to Enhance Gut Health During Recovery
Taking proactive steps to improve gut health can support addiction recovery and overall well-being. By making targeted lifestyle changes, individuals can restore gut balance, reduce inflammation, and enhance brain function. Here are practical strategies to optimize gut health during recovery:
1. Stress Management
Practice mindfulness, meditation, or yoga to reduce stress and inflammation. Engage in hobbies and activities that promote relaxation and mental clarity, such as journaling or art therapy.
2. Sleep Hygiene
Maintain consistent sleep patterns to support gut and mental health. Create a bedtime routine, avoid screens before bed, and ensure a comfortable sleep environment.
3. Physical Activity
Exercise promotes gut motility and reduces inflammation. Activities like walking, swimming, and yoga can also help regulate mood and stress levels.
4. Balanced Diet
Follow a diet rich in fiber, fermented foods, and lean proteins. Incorporate whole foods and avoid processed sugars and fats that can harm gut health.
5. Professional Support
Work with nutritionists and addiction specialists to personalize dietary and recovery plans. Participate in therapy programs that address mental and physical health as interconnected aspects of recovery, including dual diagnosis programs for treating co-occurring disorders.
Healing the Body and Mind With Lumina Recovery
The relationship between gut health and addiction reveals how interconnected physical and mental health can be. Addressing gut health through diet, stress management, and therapies can create a foundation for long-term recovery.
At Lumina Recovery, we offer dual diagnosis treatment to address both addiction and mental health conditions like anxiety and depression. We also provide medication-assisted treatment (MAT) to support recovery and reduce withdrawal symptoms. These services align with promoting gut and brain health as part of a holistic recovery approach.
Take the first step toward better health and recovery today. Contact Lumina Recovery to learn how we can support your journey.
Sources:

Benefits of Specialized Addiction Treatment Programs for Seniors
Addiction among seniors is a growing problem that often goes unnoticed. As people age, life changes such as retirement, loss of loved ones, and chronic pain can increase the risk of substance misuse.
Despite these challenges, senior addiction is frequently misdiagnosed or overlooked, leaving many without access to the specialized treatment programs they need. Specialized senior addiction treatment provides tailored care to address the physical, emotional, and social needs of older adults, offering a path to lasting recovery.
The Growing Issue of Addiction in Seniors
Did you know that nearly 1 million adults aged 65 and older struggle with substance abuse in the United States?1
While addiction is often associated with younger people, it is a growing concern among seniors. Unfortunately, addiction in older adults frequently goes unnoticed, as symptoms may be mistaken for signs of aging. This oversight can lead to delayed treatment and worsening health outcomes.
Key Statistics
- Approximately 7 million seniors, or 4.6% of adults aged 65 and older, met the criteria for alcohol use disorder within the past year.2
- Adults aged 65 and older accounted for 38% of all alcohol-related deaths in 2020 and 2021.2
- Over 80% of older adults reported taking at least one prescription medication daily, and nearly half of seniors used more than five medications or supplements regularly.1
Why Seniors Are at Risk
Several factors contribute to addiction among seniors, including:
- Retirement and lifestyle changes. Loss of daily structure can lead to boredom or depression.
- Grief and loss. The death of a spouse, close friend, or family member can trigger substance abuse.
- Chronic pain management. Long-term prescriptions for pain can lead to dependency.
- Loneliness and isolation. Reduced social interactions may increase the risk of turning to substances for comfort.
Misdiagnosis Problem
Addiction symptoms in seniors, such as confusion, fatigue, and forgetfulness, are often misattributed to natural aging or medical conditions like dementia. This oversight can delay intervention, ultimately making older adult addiction treatment more challenging.
Unique Challenges Seniors Face in Addiction Recovery
Older adults face unique barriers to addiction recovery. Their physical health, emotional stability, and social environments can complicate treatment, making specialized care essential for long-term success.
Physical Health Concerns
Many seniors face chronic illnesses such as diabetes, arthritis, or heart disease, which complicates detox and recovery.
Older adults often have weakened immune systems, making treatments like detox difficult.
Medication interactions are a major concern as many seniors take multiple prescriptions, increasing the likelihood of harmful drug interactions.
Mental and Emotional Factors
Mental health concerns like depression and anxiety are prevalent and must be addressed alongside addiction.
Cognitive decline, including memory issues, can impact treatment adherence and recovery success.
Social Barriers
The stigma around addiction may make seniors feel embarrassed about seeking senior addiction treatment.
Isolation and lack of social support can hinder motivation to recover.
Mobility issues and limited transportation options may prevent regular attendance at therapy or support groups.

5 Key Benefits of Specialized Senior Addiction Treatment Programs
Specialized older adult addiction treatment offers age-specific services designed to help seniors safely recover while addressing their unique health and emotional needs. These programs focus on long-term success through tailored support and therapies.
1. Tailored Medical Support
Programs designed for seniors focus on age-specific detox protocols and management of prescription medications to avoid harmful interactions.
2. Emotional and Mental Health Services
Therapy options include counseling, cognitive behavioral therapy (CBT), and trauma-informed care tailored to older adults.
3. Peer Support Networks
Group therapy sessions allow seniors to connect with others facing similar challenges, reducing feelings of isolation.
4. Flexible Treatment Plans
Seniors can choose from inpatient, outpatient, or home-based programs to fit their specific needs and preferences.
5. Focus on Holistic Health
Many programs incorporate yoga, meditation, and nutritional counseling to promote overall wellness.
How Specialized Programs Improve Long-Term Recovery
Long-term recovery requires ongoing support and personalized care. Senior addiction treatment programs offer aftercare plans, family involvement, and community engagement to create a strong foundation for sobriety.
Personalized Aftercare Plans
Seniors benefit from individualized relapse prevention strategies and ongoing support to maintain sobriety.
Family Involvement
Family therapy sessions help loved ones learn how to provide support and create a positive recovery environment.
Community Engagement
Seniors are encouraged to participate in senior-friendly support groups, volunteer work, or social clubs to maintain purpose and connection.
How to Choose the Right Senior Addiction Treatment Program
Finding the right older adult addiction treatment program is critical for success. Seniors and their families should evaluate programs carefully to ensure they meet specific needs.
What to Look For
- Ensure the program is licensed and accredited, with experienced staff specializing in senior care.
- Look for customized treatment plans that address physical and mental health needs, including chronic illnesses and co-occurring disorders.
- Evaluate medical detox services that cater specifically to seniors.
- Confirm access to dual diagnosis treatment to address mental health issues like depression and anxiety.
- Assess the availability of alternative therapies such as yoga, meditation, and nutritional counseling.
- Check whether the program offers aftercare support and relapse prevention strategies to sustain long-term recovery.
Questions to Ask Providers
- What therapies and services are offered?
- How are medical conditions and medications managed?
- Are family members involved in the treatment process?
Start Your Path to Healthier Living With Lumina Recovery
Addiction among seniors is a serious issue, but recovery is possible with the right support. At Lumina Recovery, our specialized programs for seniors and older adults offer detox services to help seniors safely withdraw from substances and dual diagnosis programs to address co-occurring mental health conditions. These programs ensure seniors receive comprehensive care that targets both addiction and underlying emotional health.
If you or a loved one is struggling, don’t wait to get help. Reach out to Lumina Recovery today to start the journey toward a healthier, substance-free life.
Sources:

What Is Medication-Assisted Treatment (MAT) for Addiction Recovery?
Addiction recovery can be an uphill battle, often requiring more than just willpower or determination. Many individuals face overwhelming cravings, painful withdrawal symptoms, and emotional challenges.
Overcoming these hurdles requires a comprehensive treatment approach. Medication-assisted treatment (MAT) is one such solution that has gained widespread acceptance in addiction recovery.
What Is MAT (Medication-Assisted Treatment)?
MAT is a treatment method designed to support individuals recovering from substance use disorders by using FDA-approved medication with behavioral therapies. The primary goal is to provide a “whole-patient” approach to treatment.
This holistic approach not only reduces cravings and withdrawal symptoms but also improves long-term recovery outcomes. MAT gives people the tools they need to break free from addiction and rebuild their lives.
Historically, MAT emerged as a response to the opioid epidemic, which began in the mid-20th century. Methadone was the first medication approved for treating opioid addiction in the 1960s. Over the years, research has expanded, leading to more medications and refined treatment protocols. Today, MAT is widely recognized as a life-saving option for those struggling with addiction.1
The role of MAT has continued to grow as it has become an effective treatment not only for opioid use disorder but also alcohol use disorder. It has become a central component of modern addiction treatment programs, reducing stigma and increasing access to care.
How MAT Works
The biological mechanisms behind MAT focus on stabilizing brain chemistry. Substance abuse often alters the brain’s reward system, making it difficult for individuals to feel normal without drugs or alcohol.
MAT medications work by:
- Blocking the euphoric effects of substances
- Reducing cravings
- Easing withdrawal symptoms
- Restoring balance in brain chemistry
This allows individuals to focus on therapy, counseling, and rebuilding their lives without the constant burden of cravings. MAT acts as a bridge, helping people make the transition from addiction to sobriety with medical and emotional support in place.
Medications Used in MAT
Medication-assisted treatment (MAT) uses specific medications to address withdrawal symptoms, cravings, and brain chemistry imbalances caused by addiction. These medications are carefully selected based on the substance being treated and are paired with counseling and therapy for a comprehensive approach. Below is a breakdown of commonly used medications for opioid and alcohol use disorders.
For Opioid Use Disorder
- Methadone: Reduces withdrawal symptoms and cravings while blocking the effects of opioids.
- Buprenorphine: A partial opioid agonist that helps alleviate withdrawal and reduces cravings.
- Naltrexone: Blocks opioid receptors, preventing users from experiencing a high.
For Alcohol Use Disorder
- Acamprosate: Helps restore brain chemistry disrupted by alcohol use and reduces cravings.
- Disulfiram: Creates unpleasant effects (nausea, headache) when alcohol is consumed, deterring use.
- Naltrexone: Reduces alcohol cravings and blocks its pleasurable effects.
These medications are tailored to each individual’s needs, and medical professionals carefully monitor their use to ensure safety and effectiveness.
5 Benefits of MAT
MAT offers a well-rounded approach to addiction recovery by addressing both physical and psychological challenges. It not only alleviates withdrawal symptoms and reduces cravings but also supports long-term recovery through improved treatment retention and relapse prevention.
MAT has proven to be a highly effective treatment approach, offering numerous benefits including:
- Improved treatment retention. Patients receiving MAT are more likely to stay in treatment programs.
- Reduction in illicit substance use. MAT reduces the urge to use illicit drugs, promoting abstinence.
- Lower risk of overdose. Medications like naloxone can reverse overdoses, while others reduce the likelihood of overdose by curbing cravings.
- Better quality of life. Patients often report improved relationships, employment stability, and emotional well-being.
- Reduced relapse rates. MAT lowers the chances of relapse compared to non-medication approaches.

Integrating Behavioral Therapies
While medications address physical dependency, behavioral therapies tackle emotional and psychological aspects of addiction.
Counseling sessions and support groups provide a platform for them to explore underlying issues, learn coping strategies, and develop healthy habits. Approaches such as dialectical behavior therapy (DBT) and hypnotherapy complement MAT by addressing thought patterns and building motivation for change.
MAT programs often integrate individual therapy, group counseling, and family therapy to ensure patients receive well-rounded support. These therapies empower individuals to develop healthier behaviors and address trauma, stress, or mental health challenges that may contribute to addiction.
Addressing Common Misconceptions
Despite its proven effectiveness, MAT is often misunderstood. Misconceptions and stigma can create barriers to seeking help, leaving many individuals without access to this life-changing approach. It is important to clarify these myths and provide accurate information to support informed decisions about addiction recovery.
- Myth: “MAT replaces one addiction with another.”
Reality: MAT stabilizes brain chemistry without causing a high, allowing patients to function normally. - Myth: “Recovery should be medication-free.”
Reality: MAT is a medically proven treatment, just like medications for diabetes or high blood pressure. - Myth: “MAT is only for short-term use.”
Reality: MAT can be used for as long as necessary, including long-term maintenance to prevent relapse.
By addressing these misconceptions, more individuals can access the support they need without fear of judgment.
Recent Advancements in MAT
As MAT continues to evolve, recent advancements have further improved its accessibility, effectiveness, and overall patient outcomes. New medications, such as long-lasting injectables, provide extended relief from cravings and withdrawal symptoms, reducing the need for daily doses and improving adherence to treatment plans.2
Telemedicine options have also expanded, allowing patients to consult with healthcare providers virtually, making MAT more accessible to those in rural or underserved areas. In addition, digital tools and mobile apps have emerged to help individuals track progress, set goals, and access support resources in real time.
These innovations ensure that MAT remains a flexible and evolving approach to addiction recovery, meeting the needs of patients in an increasingly connected world.
Find Recovery Solutions With Lumina Recovery
Medication-assisted treatment (MAT) has revolutionized addiction recovery by addressing both physical and emotional challenges. It combines FDA-approved medications with evidence-based therapies, offering individuals a comprehensive path to lasting recovery.
Lumina Recovery specializes in MAT programs along with dual diagnosis treatment to support co-occurring mental health conditions. These integrated approaches ensure clients receive personalized care that promotes long-term success.
If you or a loved one is ready to take the next step, contact Lumina Recovery today for a personalized treatment plan.
Sources:
Additional Resources
Once you have completed your rehabilitation program at one of our drug and alcohol treatment centers, you should try to surround yourself with people who can encourage you to stay sober. Many people find that support groups are the best source of encouragement. You can find hundreds of support groups and meetings in your community. Our drug addiction treatment centers stress the importance of personal chemical dependency resources, especially when you are new to sobriety. Below are various addiction and mental health resources for people in recovery who want additional support.
Christian Addiction Recovery Resources
Our substance abuse services aren’t limited to specific programs, but rather we believe in the importance of incorporating faith-based programs to promote spiritual healing, like our Faith in Recovery program.
With that said, below are some faith-based addiction recovery resources that could help you in your spiritual healing from addiction:
- Battlefield of the Mind by Joyce Meyer
- Boundaries by Dr. Henry Cloud & Dr. John Townsend
- Christian Families in Recovery: A Guide for Addiction, Recovery, and Intervention Using God’s Tools of Redemption by Robert and Stephanie Tucker
- Club New Life Christian Ministry for Addiction and Recovery
- Lost & Found: Recovery in Christ by Bruce Stanley
- Overcoming Emotional Obstacles through Faith: Navigating the Mind Field by Anthony Acampora, Director of Banyan’s Faith in Recovery Program
- The Case for Christ by Lee Strobel
Mental Health Resources for Recovery
Lumina Recovery consist of both mental health and substance abuse treatment facilities, meaning we offer mental health resources as well as chemical dependency resources. What’s more, addiction often co-occurs with mental illness, making these resources ever more important.
Below are some resources for mental health recovery that can help you or your loved one:
- This Emotional Life video series
- No Kidding, Me 2!! with Joe Pantoliano
- Dare: The New Way to End Anxiety and Stop Panic Attacks by Barry McDonagh
- Pleasure Unwoven: An Explanation of the Brain Disease of Addiction by Kevin McCauley
- Declutter Your Mind: How to Stop Worrying, Relieve Anxiety, and Eliminate Negative Thinking by S.J. Scott and Barrie Davenport
Call Us Today – (877) 716-7515

