In the journey towards recovery from opioid addiction, choosing the right medication-assisted treatment (MAT) is a crucial step. Two commonly prescribed medications in MAT are methadone and Suboxone.
Both have been proven effective but differ in their mechanisms, side effects, and administration. Understanding methadone vs. Suboxone can help individuals and their loved ones make informed decisions in their recovery process.
What Is Methadone?
Methadone is an extended-release opioid medication that supports individuals with opioid use disorder by alleviating cravings and easing withdrawal symptoms.
It works by acting on the same opioid receptors as drugs like heroin and prescription painkillers but in a controlled and sustained manner, preventing the intense highs and lows associated with opioid abuse. When used as part of a medically supervised treatment plan, methadone helps stabilize individuals and allows them to focus on their recovery.1
Unlike illicit opioids, methadone does not cause the same level of euphoria when taken as prescribed. It is dispensed in liquid, tablet, or wafer form through licensed treatment programs. Because of its potency and potential for misuse, methadone treatment requires close medical monitoring. However, when administered properly, it is a highly effective tool for opioid addiction recovery, allowing individuals to regain stability and improve their overall quality of life.
What Is Suboxone?
Suboxone treatment is a medically prescribed approach for managing opioid dependence. It contains buprenorphine, a partial opioid agonist that minimizes cravings and alleviates withdrawal symptoms, along with naloxone, an opioid antagonist that helps prevent misuse by counteracting opioid effects. This combination makes Suboxone an effective and safer alternative to full opioid agonists.2
Unlike methadone, Suboxone has a ceiling effect, meaning that increasing the dose beyond a certain point does not intensify its effects. This reduces the risk of overdose while still providing relief from opioid dependence.2
Additionally, Suboxone is typically prescribed in film or tablet form and can be taken at home under a doctor’s supervision, making it a more convenient option for many individuals.
Because of its partial agonist nature, Suboxone is less likely to cause the same level of physical dependence as full opioids. However, careful medical supervision and a structured treatment plan are still required to ensure its effectiveness in supporting long-term recovery.
What Is the Difference Between Methadone and Suboxone?
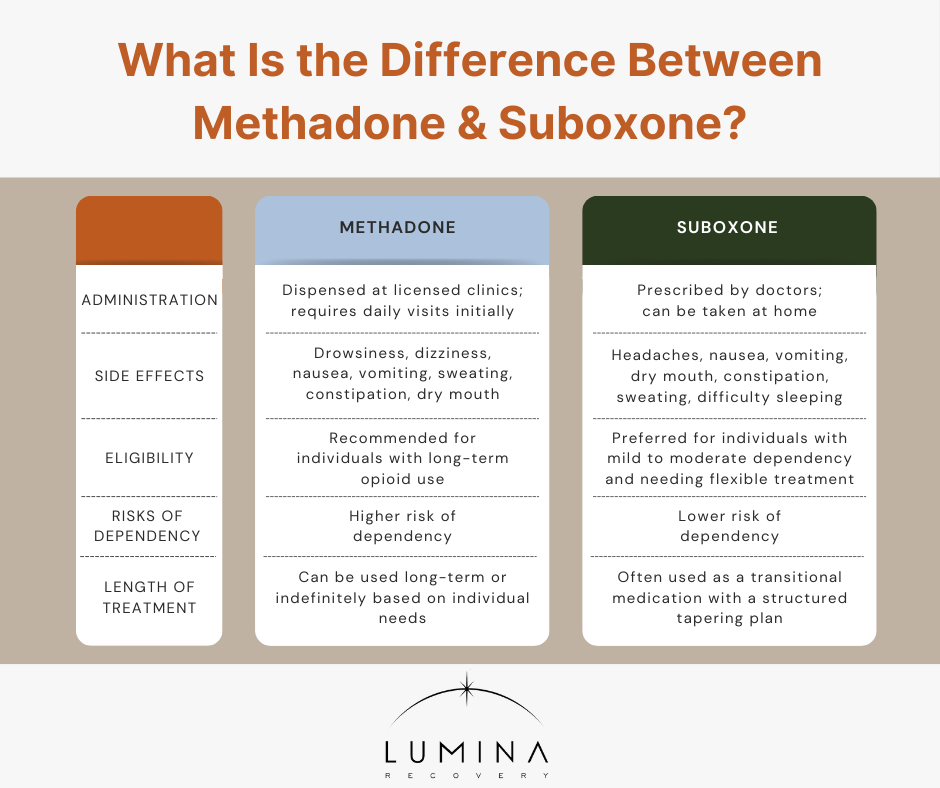
Methadone and Suboxone are both medications used to treat opioid use disorder, but the difference between Suboxone and methadone lies in their administration, side effects, eligibility, risks of dependency, and duration of treatment. Comparing Suboxone vs. methadone can help individuals determine which medication aligns best with their recovery needs.
Administration
Methadone is typically provided in liquid, tablet, or wafer form and must be dispensed through certified opioid treatment programs. In the early stages of treatment, patients are usually required to visit a clinic daily to receive their doses under medical supervision. This strict regulation helps prevent misuse and ensures proper dosage adjustments. As patients demonstrate progress and stability, they may receive take-home privileges.
Suboxone offers a more flexible treatment option. It is usually prescribed in film or tablet form and can be taken at home. Patients typically begin Suboxone treatment under medical supervision, either in a clinic or a private doctor’s office. Once stabilized, they can receive prescriptions to be filled at a pharmacy, similar to other medications.
Side Effects
Methadone may cause a range of side effects, including drowsiness, dizziness, nausea, vomiting, sweating, constipation, and dry mouth. Some individuals may experience weight gain or sexual dysfunction. More severe side effects include respiratory depression, particularly when the dosage is not properly adjusted or when methadone is combined with other substances.1
Suboxone also has potential side effects, including headaches, nausea, vomiting, dry mouth, constipation, sweating, and difficulty sleeping. Some individuals may experience swelling in the extremities or a numb sensation in the mouth due to the film form of the medication. Unlike methadone, Suboxone has a lower risk of respiratory depression, making it a safer option in overdose situations.2
Eligibility
Methadone is generally recommended for individuals with a long history of opioid addiction, particularly those who have not succeeded with other treatments. It is suitable for patients who require a highly structured treatment plan and who can commit to regular visits at a methadone clinic. Since methadone has a higher potential for dependency, it is often prescribed for individuals who need close medical supervision and additional support services.
Suboxone is often prescribed to individuals with mild to moderate opioid dependency or those transitioning from stronger opioids. It is a preferred option for people who require a more flexible treatment plan and can manage their recovery with outpatient care.
Risks of Dependency
Methadone is effective for managing withdrawal symptoms and cravings, but it has a high potential for dependency. If not properly managed, patients can develop physical dependence, and withdrawal symptoms can be severe if the medication is stopped suddenly.
Suboxone contains buprenorphine which reduces cravings and withdrawal symptoms while having a lower risk of dependency compared to methadone. The presence of naloxone further reduces misuse potential by discouraging intravenous use. While Suboxone can still lead to physical dependence, its partial agonist properties result in a milder withdrawal process than full opioids like methadone.
Length of Treatment
Methadone treatment duration varies significantly depending on the individual’s needs. Some people may require long-term or even lifelong methadone maintenance therapy to manage opioid dependence effectively. Others may use methadone as a step-down treatment before transitioning to an opioid-free life.
The length of Suboxone treatment depends on the individual’s recovery progress. Some patients use Suboxone for a short period as part of a tapering strategy, while others may require long-term maintenance. Methadone can be used indefinitely, whereas Suboxone is often used as a transition medication to gradually reduce opioid dependence.
Frequently Asked Questions (FAQs)
Is Suboxone the same as methadone?
No, Suboxone and methadone are different medications used to treat opioid use disorder. Methadone is a full opioid agonist, while Suboxone contains buprenorphine (a partial agonist) and naloxone, which helps reduce misuse potential.
Can you take methadone and Suboxone together?
No, taking methadone and Suboxone together is not recommended. Suboxone contains naloxone, which can precipitate opioid withdrawal if taken while methadone is still active in the system.
Is Suboxone stronger than methadone?
Methadone is generally considered stronger because it is a full opioid agonist, whereas Suboxone is a partial agonist with a ceiling effect that limits its opioid-like effects. However, the effectiveness of each medication depends on the individual’s needs and treatment goals.
Start Opioid Addiction Treatment Today With Lumina Recovery
Methadone and Suboxone are both effective in treating opioid use disorder, but they differ in administration, side effects, eligibility, dependency risks, and treatment duration. Choosing the right option depends on individual needs and lifestyle factors.
At Lumina Recovery, we offer medication-assisted treatment (MAT) and specialized opioid use disorder treatment to help individuals safely recover from opioid addiction. Our expert team provides comprehensive care to support long-term sobriety and overall well-being.
If you or a loved one is struggling with opioid addiction, contact Lumina Recovery today to learn how our personalized treatment plans can help you take the first step toward recovery.
Sources: