
Our Addiction Resources
Navigating the world of addiction and recovery can be overwhelming. We’re here to provide clear, compassionate education and guidance. From practical advice for maintaining sobriety to informational guidance on the long-term effects of substance abuse, our content is a beacon of hope and understanding.
Our Team is Ready are ready to take your call
Call us Today!
or we can call you. Fill out form below
Our Blog

Side Effects and Signs of Hydrocodone Addiction
Hydrocodone is a prescription opioid used to treat severe, around-the-clock pain and is classified as a Schedule II controlled substance in the United States. Due to the significant risk of drug abuse and addiction to hydrocodone, it should not be used to treat occasional moderate or severe pain. 1
Known on the streets as Vike and Watson-387, hydrocodone is commonly encountered as small pills but can also be found in syrup form. 2 Understanding hydrocodone’s characteristics, potential for addiction, and its side effects is crucial for individuals taking the medication and their loved ones.
Hydrocodone’s Addiction Potential
Hydrocodone works by binding to opioid receptors in the brain and spinal cord, which are part of the central nervous system. This binding alters pain perception and can induce feelings of pleasure or euphoria, contributing to its abuse potential.
Regular long-term use, even as prescribed, can lead to physical dependence and tolerance, where more of the drug is needed to achieve the same effects, setting a foundation for potential substance abuse. 3
Identifying Signs of Hydrocodone Addiction
Recognizing the signs and symptoms of hydrocodone addiction can help in seeking intervention early, which is critical for successful recovery. Signs of hydrocodone addiction can include: 3
- Increased tolerance. One of the first signs of abusing hydrocodone is needing increasingly higher doses of hydrocodone to feel the same effects. This tolerance can develop quickly, prompting users to consume more than their prescribed dose.
- Withdrawal symptoms. As physical dependence on hydrocodone develops, opioid withdrawal symptoms can occur if the drug is not taken regularly. Symptoms may include anxiety, irritability, muscle aches, insomnia, sweating, and in severe cases, nausea and vomiting.
- Loss of control. An individual may start using more hydrocodone than intended, or for longer periods than planned. They might express a persistent desire to cut down or control use but repeatedly fail to do so.
- Time spent. A lot of time may be spent obtaining hydrocodone, using it, or recovering from its effects. This might involve visiting multiple doctors to obtain more prescriptions, a practice known as “doctor shopping.”
- Neglect of duties. With increasing preoccupation with the drug, the individual may neglect responsibilities at work, school, or home. This neglect can manifest in decreased performance and attendance, neglecting household chores, or disregarding family obligations.
- Continued use despite problems. Continued hydrocodone use despite the clear knowledge of persistent or recurrent physical or psychological problems likely to have been caused or exacerbated by the drug is a strong indicator of addiction.
- Social or recreational sacrifices. An individual might give up important social, occupational, or recreational activities because of hydrocodone use, choosing to use the drug instead of engaging in these activities.
- Risky use. The person may use hydrocodone in physically hazardous situations, such as driving or operating machinery, or in higher doses despite the known risks.
Side Effects of Hydrocodone
Many hydrocodone side effects range from mild to severe. Being aware of these side effects can help individuals and their caregivers manage the medication more effectively and recognize when medical attention may be needed.
Common Side Effects
The most frequently observed side effects of hydrocodone include: 4
- Stomach Pain: This can vary from mild discomfort to severe pain.
- Dry Mouth: Persistent dryness in the mouth.
- Tiredness: Unusual fatigue or lack of energy.
- Headache: Moderate to severe
- Back Pain: Pain located in the lower or upper back.
- Muscle Tightening: Involuntary or uncomfortable muscle contractions.
- Ringing in the Ears: Persistent noise or ringing sounds in one or both ears.
- Sleep Disturbances: Difficulty falling asleep or staying asleep throughout the night.
- Swelling: Swelling of the feet, legs, or ankles.
- Uncontrollable Shaking: Part of the body may shake uncontrollably.
- Increased Sweating: Noticeable increase in sweating without physical exertion.

Serious Side Effects
While less common, some serious side effects require immediate medical attention: 4
- Chest Pain: Any new or worsening chest pain.
- Neurological and Psychological Reactions: Symptoms like agitation, hallucinations, fever, confusion, fast heartbeat, shivering, severe muscle stiffness or twitching, loss of coordination, or diarrhea.
- Gastrointestinal and General Discomfort: Nausea, vomiting, loss of appetite, weakness, or dizziness.
- Sexual Health Issues: Problems such as inability to get or keep an erection, irregular menstruation, or decreased sexual desire.
- Cardiac Symptoms: Any changes in the rhythm or speed of the heartbeat.
- Allergic Reactions: Signs include rash, hives, hoarseness, and difficulty breathing or swallowing; swelling of the face, mouth, tongue, or throat.
- Urinary Problems: Difficult, frequent, or painful urination.
Find Support for Hydrocodone Addiction
If hydrocodone use has transitioned from therapeutic use to dependency or addiction, talking to a doctor is a critical first step. They can provide guidance, assess the level of dependency, and recommend treatment options. There are many facets to getting support for hydrocodone addiction.
Various programs offer specialized treatment for prescription opioid addiction, including inpatient and intensive outpatient settings. These programs often combine medication-assisted treatment (MAT) with counseling and behavioral therapies to help manage withdrawal symptoms and address the underlying causes of addiction.
Medication-assisted treatment (MAT) uses medications like buprenorphine, methadone, and naltrexone to reduce cravings and withdrawal symptoms, making it easier to focus on recovery.
Cognitive behavioral therapy (CBT) and other therapeutic approaches can help individuals change their thinking and behavior related to drug use. Therapists can also help address co-occurring disorders such as anxiety or depression.
Addiction affects not just the individual but also their family. Family therapy can help improve communication, resolve conflicts, and support the entire family’s journey through recovery.
Groups such as Narcotics Anonymous (NA) or other community support groups provide peer support, which is invaluable during recovery. These groups offer a platform to share experiences and coping strategies in a supportive and understanding environment.
Get Help for Hydrocodone Addiction With Lumina Recovery
Lumina Recovery provides prescription drug and opioid treatment for those looking for support at any stage in their recovery journey.
If you or someone you love is struggling with substance abuse, reach out for professional help. Addiction is a treatable condition, and with the right support, recovery is achievable.
Sources:
- https://www.mayoclinic.org/drugs-supplements/hydrocodone-oral-route/description/drg-20084881
- https://www.nihlibrary.nih.gov/resources/subject-guides/opioids/street-commercial-names
- https://www.healthline.com/health/understanding-hydrocodone-addiction#causes
- https://medlineplus.gov/druginfo/meds/a614045.html#side-effects

What Is the Relationship Between Outpatient Treatment and Sober Living?
Transitioning from the structured environment of an inpatient rehab program to the unpredictability of everyday life can be daunting. Many people feel fragile after achieving sobriety, and the thought of facing daily challenges without constant support can be overwhelming. This uncertainty is one reason why relapse is so common in recovery. However, with ongoing support and guidance, the risk of relapse can be significantly reduced.
A robust aftercare support system is crucial in early recovery. Sober living houses (SLHs) offer a safe and supportive environment that complements outpatient treatment. SLHs foster a sense of community, promoting abstinence and peer support, while outpatient programs provide structured therapy and counseling.
By combining these elements, individuals can receive a holistic approach to recovery that not only helps prevent relapse but also supports their journey toward a substance-free life.
What Is Outpatient Treatment?
Outpatient treatment refers to therapeutic services that allow individuals to receive care for substance abuse and addiction while living outside of a treatment facility. Unlike inpatient programs that require patients to stay onsite, outpatient treatment provides flexibility, enabling individuals to maintain their daily routines such as work, school, or family obligations.
This type of treatment is often recommended for those who have completed an inpatient program and are looking to continue their recovery support as they reintegrate into their daily lives.
Outpatient treatment varies in intensity and structure, but typically includes individual and group counseling, education about substance abuse, and support for managing relapse. Among the options available, partial hospitalization programs (PHP) and intensive outpatient programs (IOP) stand out as two primary forms of care.
Partial hospitalization programs (PHP) are the most intensive form of outpatient treatment. PHPs typically require individuals to attend therapy sessions for several hours each day, up to five to seven days a week. These programs are suitable for those who need substantial support and monitoring, yet have a stable living situation.
Intensive outpatient programs (IOP) are less demanding than PHPs, typically requiring attendance at therapy sessions for a few hours each day, three to four days a week. IOPs are ideal for individuals transitioning from a PHP or those with moderate support needs, allowing more flexibility to engage in everyday activities while still receiving comprehensive therapy.
Outpatient programs are generally more affordable than inpatient programs, making them accessible to a broader range of people. They play a crucial role in supporting lasting recovery and facilitating reintegration into society.
What Is Sober Living?
Sober living homes, also called halfway houses or recovery residences, provide a structured and supportive environment for those not yet ready for full independence.
These homes offer a transitional space with more support and accountability than individuals might have on their own. SLHs maintain structure through rules like curfews, scheduled meal times, and required household chores, creating a balanced and stable atmosphere.
SLHs provide a safe space for residents to rebuild their lives at their own pace, free from drugs and alcohol. Regular check-ins, community meetings, and support groups create a sense of community, encouraging the sharing of experiences and achievements, and fostering camaraderie among residents.
This peer support network is crucial for long-term recovery, offering both empathy and motivation and often serving as a lasting source of support even after residents move out.
Residents are encouraged to find employment, pursue education, or engage in volunteer work to build life skills and a sense of responsibility—key elements for maintaining long-term sobriety. Many SLHs also offer additional support services, such as job coaching and educational resources, to assist residents in reintegrating into society.
How Are These Two Options Related to Each Other?
Combining sober living homes with outpatient rehab programs offers an increased level of support. This integrated approach provides a dual layer of care—the structured, substance-free environment of a sober living home, along with the personalized therapeutic services of outpatient programs.
This option is designed for those who need extra support and accountability, especially in the early stages of sobriety, after an intensive inpatient program, or when dealing with repeated relapses. This combination creates a supportive ecosystem that fosters recovery in several ways, including:
- Stability and Structure: Sober living homes offer a stable environment with clear rules and expectations, while outpatient programs provide ongoing therapy and support. This balance allows individuals to continue their recovery journey in a setting that encourages accountability without the rigidity of inpatient treatment.
- Flexibility and Independence: Sober living homes provide structure, while outpatient programs offer the flexibility to attend therapy and counseling while managing daily responsibilities. This flexibility helps individuals rebuild their lives, pursue employment or education, and gradually transition to independent living.
- Resource Accessibility: Sober living homes often connect residents with valuable resources such as job opportunities and educational programs. Outpatient programs complement this by offering therapy, support groups, and other services to strengthen coping skills and resilience.
- Reduced Risk of Relapse: By providing a safe, substance-free environment alongside consistent therapeutic support, this approach helps reduce the risk of relapse. The combination of structure and ongoing therapy enables individuals to develop the skills and emotional resilience needed to maintain long-term sobriety.
Together, sober living homes and outpatient programs create a comprehensive recovery strategy that addresses both the physical and emotional aspects of overcoming addiction.
This approach not only supports individuals during the critical transition from inpatient treatment to independent living, but it also provides the resources and flexibility to help them successfully reintegrate into society. It’s a compassionate and effective path toward lasting recovery.
Why Choose Lumina Recovery for Outpatient Treatment and Sober Living?
At Lumina Recovery, we believe everyone has the strength to overcome addiction and achieve lasting recovery. Our holistic approach goes beyond treating addiction symptoms, addressing your physical, emotional, and mental health. Our mission is to guide you toward long-term sobriety with compassion and evidence-based care.
We know that each recovery journey is unique. Our integrated sober living and outpatient programs offer flexibility, allowing us to adjust the level of care to meet your specific needs. This setup is ideal for those who benefit from the structure and community of sober living while attending outpatient treatment.
Whether you need a combination of outpatient care and sober living, or another tailored treatment plan, we’re here to help. Discuss your situation with our team, and together, we’ll create a recovery plan that suits your unique needs.
Contact us today to learn how we can support your journey to wellness.

Symptoms and Signs of Codeine Addiction
Among the various substances that can grip a person, codeine stands out as a common prescription drug to treat mild to moderate pain. Unfortunately, its accessibility in drugs like cough syrup contributes to its high potential for abuse.
Whether you are a patient addicted to codeine for treating pain, someone concerned about a loved one, or just seeking knowledge, it is essential to recognize the signs of codeine addiction and understand both the immediate and long-term effects of codeine use.
Generic and Brand-Name Codeine
Codeine is a commonly abused opioid pain reliever that is available in both generic and brand-name forms.
Generic codeine is available under its chemical name, “codeine,” without any brand association. Pharmacies may stock generic codeine in various formulations, such as tablets, capsules, and liquids, which are used to ease severe pain and coughing.
Several brand-name drugs include codeine, either as a single active ingredient or in combination with other medications like acetaminophen or ibuprofen. These combinations are intended to enhance pain relief or tackle multiple symptoms, such as a fever. Some of the well-known brand-name drugs containing codeine include Tylenol with Codeine, Robitussin A-C, and Promethazine with Codeine.
Street names for the drug include Cody, Schoolboy, Lean, Sizzurp, and Purple Drank.1
Signs and Symptoms of Codeine Addiction
Recognizing the signs of codeine abuse is critical for timely intervention. Addiction can manifest in various behavioral and physical ways, including:2
Behavioral Signs
- Compulsive Use: Using codeine more frequently or in larger amounts than intended, often with a persistent desire or unsuccessful attempts to cut down.
- Preoccupation With Codeine: Spending a substantial amount of time obtaining, using, or recovering from the effects of codeine.
- Neglect of Duties: Ignoring or reducing engagement in social, occupational, or recreational activities due to drug use.
- Continued Use Despite Problems: Persisting in using codeine despite being aware of the physical or psychological problems it is causing.
- Social Isolation: Withdrawing from family and friends, and showing a reduced interest in activities previously enjoyed.
- Financial Decisions: Spending significant amounts of money on acquiring codeine, may lead to financial strain or legal issues.
- Risk-Taking Behavior: Engaging in risky behaviors, such as driving under the influence or mixing drugs, to obtain or use codeine.
Physical Signs
- Increased Tolerance: The need for progressively larger doses of codeine to feel the same effects, which is a clear indicator of developing tolerance.
- Withdrawal Symptoms: Experiencing physical or psychological symptoms such as anxiety, irritability, nausea, vomiting, and muscle pain when not using the drug.
- Drowsiness: Frequent and excessive sleepiness, a direct effect of codeine’s sedative qualities.
- Changes in Physical Appearance: Neglecting personal grooming and hygiene as a result of preoccupation with drug use.
- Constipation: A common problem among opioid users due to the effects of the drug on the digestive system.
- Respiratory Depression: Shallow or slow breathing, which can be life-threatening at high doses or when combined with other depressants.
- Pupillary Constriction: Noticeably small pupils, also known as pinpoint pupils, which is a typical response to opioid use.
Immediate Codeine Side Effects
When codeine is used, even within prescribed limits, it can cause a range of immediate short-term side effects. Understanding the short-term effects of codeine can help in recognizing misuse or overdose:3
One of the most common effects, excessive drowsiness can impair an individual’s ability to perform daily tasks safely, such as driving or operating machinery.
Dizziness and lightheadedness can affect balance and coordination, increasing the risk of falls and injuries, especially in elderly patients.Nausea and vomiting, common gastrointestinal side effects, can lead to dehydration and electrolyte imbalances if persistent.
As with many opioids, codeine reduces bowel motility, leading to constipation, which can become severe and require medical intervention if it persists.
Particularly in higher doses, codeine can impair cognitive function, leading to confusion and poor decision-making.
The feeling of euphoria that codeine can produce is a major factor in its potential for abuse, as users seek to replicate this pleasurable sensation.
Codeine can slow breathing, and in higher doses, this can become dangerous, reducing oxygen intake to critical levels.

Long-Term Side Effects of Codeine
The long-term use of codeine, particularly when abused, can lead to serious health issues that affect various systems in the body:3
Codeine often comes combined with acetaminophen (Tylenol), and prolonged use can lead to liver damage or failure due to the toxicity of acetaminophen.
Long-term use can lead to physical dependence and addiction, conditions in which the body requires the drug to function normally, and cessation leads to withdrawal symptoms.
Chronic use of codeine can cause long-term respiratory depression, reducing lung capacity and efficiency, which can be life-threatening.
Persistent use can exacerbate or trigger mental health issues such as depression and anxiety. These disorders can complicate the addiction and make treatment more challenging.
Over time, codeine use can impair cognitive abilities, affecting memory, decision-making, and problem-solving skills.
Opioids like codeine can disrupt normal hormonal balances, leading to issues such as reduced libido, infertility, and irregular menstrual cycles.
Long-term opioid use can weaken the immune system, making the body more susceptible to infections.
Getting Help for Codeine Addiction
Codeine addiction treatment involves several steps tailored to the individual’s needs. The journey often begins with professional detoxification, conducted under medical supervision to safely manage withdrawal symptoms and minimize the risk of relapse. Following detox, individuals might enter rehabilitation programs with a range of treatments including evidence-based therapies like cognitive behavioral therapy (CBT).
Medication-assisted treatment (MAT) may also be used, employing medications like buprenorphine, naltrexone, or methadone to manage codeine withdrawal symptoms and curb cravings. Family therapy is another crucial component, as addiction impacts not just the individual but the entire family.
Aftercare planning ensures ongoing support and helps maintain sobriety, involving continuous therapy, support meetings, and lifestyle adjustments. Each step in this process is crucial for a successful recovery, providing structured and supportive environments that help individuals regain control of their lives.
Find Solutions for Codeine Addiction With Lumina Recovery
Understanding codeine addiction is vital for anyone struggling or caring for someone who is. Recognizing the signs and knowing the side effects can guide necessary decisions about seeking help.
Lumina Recovery offers opioid and prescription drug treatment programs to support those on their journey toward a healthier, substance-free life. If you or a loved one is dealing with addiction, remember that help is available and recovery is possible.
Reach out to Lumina Recovery today to start on the path to a healthier, drug-free life.
Sources:

Methadone Addiction: Key Signs and Potential Side Effects
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), methadone is a schedule II controlled long-acting opioid. Methadone treatment is commonly used for long-term pain relief and opioid use disorders (OUD) in certified opioid treatment programs (OTP).1
Despite its legitimate medical uses, some individuals use methadone illicitly, obtained either through fraudulent prescriptions or from the street. Known by various street names such as Amidone, Wafer, and Chocolate Chip Cookies, this drug poses significant risks when used outside a medical context.2
Recognizing Methadone Abuse
Identifying methadone abuse requires attention to several behavioral and physical signs that may indicate misuse of the drug, especially if it’s outside a prescribed treatment plan. Some key indicators include:3
Behavioral Changes
- Increasing secrecy about activities or withdrawing from family and friends
- Unexplained borrowing or stealing money
- Skipping work, school, or neglecting home duties
- Encounters with law enforcement or legal troubles related to drug use
Physical Signs
- Constricted pupils even in dim light
- Excessive sleepiness or difficulty in sleeping
- Neglecting personal grooming or a noticeable decline in cleanliness and order
- Unexplained weight gain or loss without changes in diet or exercise habits
- Flushing, puffiness, or a generally unhealthy appearance
Side Effects of Methadone
As the National Institute on Drug Abuse reports, methadone can help prevent the negative effects of opioid withdrawals and cravings, but it’s important to note it can also cause a range of side effects with short-term use.4 Methadone side effects include:5
- Restlessness and mood changes
- Upset stomach, vomiting, constipation, and stomach pains
- Slow breathing
- Itchy skin, heavy sweating, flushing, and in severe cases, hives or a rash
- Headaches, vision problems, and drowsiness
- Dry mouth, changes in sleep patterns, appetite fluctuations, and sexual problems
- Weight gain
There are more serious side effects where medical attention should be sought immediately:5
- Trouble breathing, a hoarse voice, or trouble swallowing
- Swollen lips, tongue, throat, or face, which can be signs of a severe allergic reaction
- Chest pain or a rapid heartbeat
- Hallucinations, confusion, fainting, lightheadedness, or seizures
- Unusual menstrual periods
Risks of Methadone Use
Methadone carries specific risks that can affect individuals based on their health status and history. It’s crucial to inform your doctor if you have any of the following conditions:5
- Heart disease or a heart rhythm disorder
- Any breathing problems or lung disease
- History of head injuries, brain tumors, or seizures
- Liver or kidney disease, and problems with your gallbladder, pancreas, or thyroid
- Issues related to urination or if you are taking sedatives
Drug Interactions
Methadone can interact with various drugs, which can exacerbate its effects or increase risks:5
- Other opioids and narcotics
- Sedatives and medications that affect breathing
- Drugs altering serotonin levels
Always inform your healthcare providers about any medications you are currently taking to avoid adverse interactions.
Dependency and Tolerance
Methadone can lead to dependency and tolerance. Over time, you might need higher doses to achieve the same pain relief effects, known as tolerance. Dependency occurs as your brain gets accustomed to the relief methadone provides, leading to withdrawal symptoms if usage stops suddenly.
Overdose Risk
Changing your medication amount without talking to a doctor can be very risky and cause an overdose, which can be deadly. Signs of an overdose include:2
- Slow, shallow breathing and weak pulse
- BIue-tinted lips and fingernails
- Clammy skin
- Stomach spasms
- Convulsions
- Coma
Impact of Methadone on the Brain and Body
Methadone mimics opiate effects on the brain and body, but its impact varies significantly with controlled versus uncontrolled use. In the brain, methadone binds to opioid receptors which are normally targeted by stronger narcotics like heroin. This binding helps reduce the cravings and withdrawal symptoms associated with opioid addiction, facilitating recovery in a medical setting.
However, this same mechanism can lead to addiction if methadone is misused, as the brain begins to rely on methadone for achieving normal function. This dependency can alter emotional stability, cognitive functions, and even personal behavior, driving the cycle of addiction deeper.
Physiologically, methadone slows the body’s systems, notably affecting the respiratory and cardiovascular systems. It can lower breathing and blood pressure, which can be helpful in moderation but harmful if used incorrectly.
Gastrointestinal motility is often reduced, leading to issues like constipation. Over time, these physical effects can compound, leading to significant health problems that require medical attention.
Overcoming Methadone Addiction
Recovering from methadone addiction involves a comprehensive approach that addresses both the physiological and psychological aspects of dependency. Typically, the process begins with a medically supervised detoxification, where the dose of methadone is gradually reduced under close medical supervision to mitigate withdrawal symptoms effectively.
Following detox, long-term treatment options include therapy and counseling, which are vital for addressing the underlying causes of addiction. Cognitive behavioral therapy (CBT), group therapy, and other forms of counseling can help modify the behaviors and thought patterns that contribute to substance abuse.
Addressing lifestyle factors such as diet, exercise, and stress management plays an essential role in recovery too. Creating a good routine and exercising regularly can make you feel better mentally and physically, helping you recover overall.
Get Help for Methadone Addiction With Lumina Recovery
Understanding the signs and effects of methadone abuse is vital for individuals and their loved ones to recognize the need for intervention and treatment. Methadone, while beneficial in controlled doses and medical environments, can lead to serious personal and health issues when abused.
Lumina Recovery provides initial detox and therapy options as part of our opioid and prescription drug addiction treatment programs. If you or a loved one is struggling with methadone addiction, it is important to seek professional help to address both the physical and psychological aspects of addiction.
Reach out to Lumina Recovery for compassionate and effective help.
Sources:
- https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/methadone
- https://www.dea.gov/factsheets/methadone
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/opioid-use-disorder
- https://nida.nih.gov/publications/research-reports/medications-to-treat-opioid-addiction/how-do-medications-to-treat-opioid-addiction-work
- https://www.webmd.com/mental-health/addiction/what-is-methadone

OxyContin Addiction Signs, Risk Factors, and Steps for Help
OxyContin is a brand-name prescription opioid containing oxycodone, commonly prescribed for severe pain management. While effective for short-term relief, its potent narcotic properties make it highly addictive, even when taken as directed.
OxyContin impacts the nervous system and brain by altering how they respond to pain, creating a euphoric and calming effect. Over time, individuals may develop both physical and psychological dependence, leading to addiction.
Understanding the signs of oxycodone abuse, symptoms of use, and addiction risks is critical for early intervention and recovery support.
OxyContin and Opioid Addiction Statistics
Opioid addiction continues to be a public health crisis in the United States. In 2020, over 48,000 people lost their lives to opioid overdoses, reflecting the devastating toll of this epidemic. Misuse of opioids is also widespread, with 3.8% of American adults abusing them each year.1
Alarmingly, opioids are involved in the majority of overdose deaths, with at least 71.8% and as many as 80% of fatalities linked to these substances. These statistics highlight the urgent need for awareness, prevention, and accessible treatment options to combat this crisis.1
OxyContin Addiction vs. Dependence
The difference between addiction and dependence is an important factor in determining effective treatment.
- Dependence: This is a physical reliance on oxycodone that develops over time as the body adapts to the drug. Dependence can result in withdrawal symptoms when use stops but does not necessarily involve compulsive behaviors.
- Addiction: Addiction is a chronic disorder characterized by compulsive drug-seeking behavior, psychological cravings, and continued use despite negative consequences. Addiction often involves significant lifestyle disruptions and difficulty controlling use.
While both conditions require treatment, addiction typically involves more extensive behavioral and psychological support to address underlying causes.
OxyContin Addiction Signs
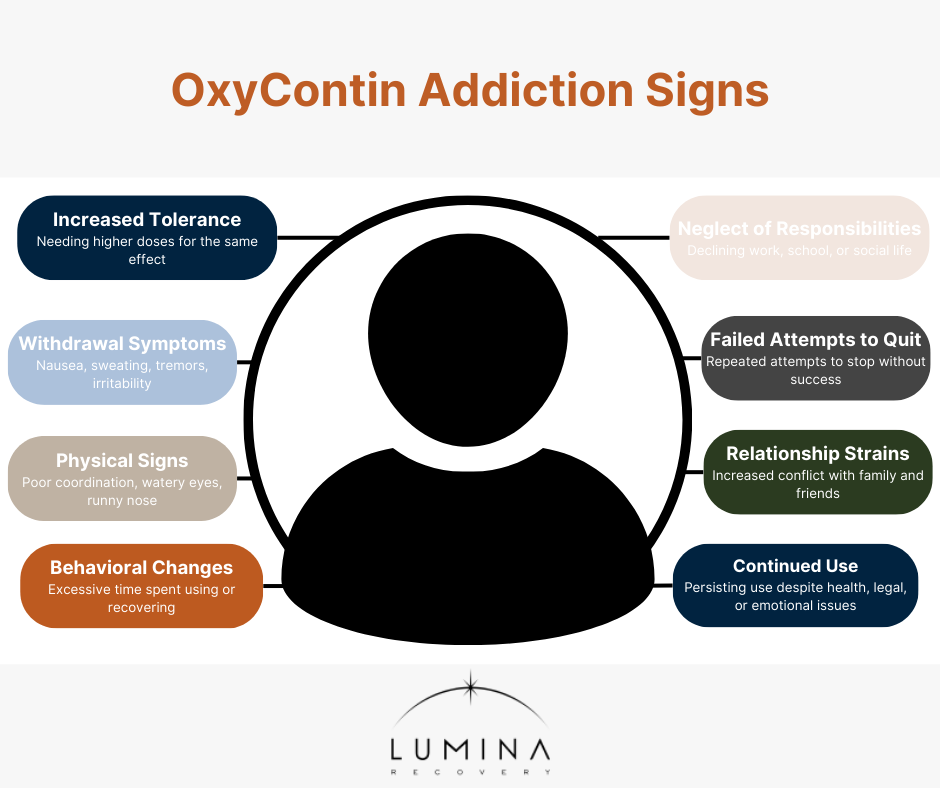
Recognizing oxycodone addiction signs early can prevent long-term harm. Key signs include:2
- Increased Tolerance: Requiring larger amounts of OxyContin to feel the same level of relief or effect as before.
- Withdrawal Symptoms: Facing symptoms like nausea, sweating, tremors, and irritability when the drug is not taken.
- Physical Signs: Impaired coordination, unexplained injuries, watery eyes, and a runny nose may indicate oxycodone symptoms of use.
- Behavioral Changes: Spending excessive time obtaining, using, or recovering from OxyContin.
- Neglect of Responsibilities: Declining performance at work or school and avoiding hobbies or social activities.
- Failed Attempts to Quit: Repeatedly trying and failing to stop using the drug.
- Relationship Strains: Increased conflicts with loved ones due to signs of oxycodone
- Continued Use Despite Problems: Persisting in use even when it causes health issues, legal troubles, or emotional distress.
Risk Factors for Oxycodone Addiction
Certain factors increase the likelihood of developing an addiction to oxycodone, including:
- Genetic Predisposition: Having a family history of substance abuse may increase the likelihood of developing similar problems.
- Environmental Influences: Growing up in an environment where drug use is common can predispose individuals to addiction.
- Mental Health Disorders: People with mental health issues such as depression, anxiety, or post-traumatic stress disorder (PTSD) may be at higher risk of addiction as they may use OxyContin as a form of self-medication.
- Chronic Pain: Individuals prescribed OxyContin for long-term pain management face a higher risk of addiction, especially without proper medical supervision.
- Previous Substance Abuse: Individuals who have a history of abusing other substances may be more likely to develop an addiction to OxyContin.
- Social and Economic Problems: Stressful life circumstances such as unemployment or lack of social support can contribute to the onset of addiction.

5 Steps to Get Help for OxyContin Addiction
Taking action is essential to overcoming oxycodone addiction symptoms and reclaiming your life. Follow these steps:
- Recognize the problem. The first step is acknowledging the issue. Educate yourself on the signs of oxy addiction and assess whether you or a loved one might be struggling.
- Seek professional detox. A medically supervised detox ensures that withdrawal symptoms are managed safely. Attempting to detox at home can be dangerous and is not recommended.
- Explore medication-assisted treatment (MAT). MAT combines FDA-approved medications like buprenorphine or methadone with counseling to reduce cravings and stabilize recovery. MAT is a proven approach to managing both the physical and psychological aspects of addiction.
- Commit to therapy. Therapy is essential for addressing the root causes of addiction. Cognitive behavioral therapy (CBT) helps individuals identify and change harmful thought patterns, while dialectical behavior therapy (DBT) supports emotional regulation. Family therapy strengthens relationships and builds a supportive recovery environment, providing a holistic approach to overcoming addiction.
- Join support groups. Support groups like Narcotics Anonymous (NA) offer peer connections and accountability. Sharing experiences with others who understand your journey can provide ongoing motivation and support.
Holistic Approaches to Recovery
Incorporating holistic therapies into your recovery plan can improve your mental and physical health, making long-term sobriety more attainable. Activities such as yoga, meditation, and regular exercise promote relaxation, reduce stress, and encourage a balanced lifestyle. These practices complement traditional treatments and enhance overall well-being.
In addition to physical wellness, holistic approaches also focus on emotional and spiritual healing. Creative outlets like art therapy, music therapy, and journaling can help individuals process emotions and build healthier coping mechanisms.
Engaging in mindfulness practices or spending time in nature can further support emotional regulation, improve self-awareness, and provide a sense of inner peace during the recovery journey.
Frequently Asked Questions (FAQs)
1. How does OxyContin make you feel?
OxyContin can create feelings of euphoria, relaxation, and pain relief, but it can also lead to drowsiness, confusion, and, with misuse, addiction.
2. What does OxyContin do to the brain?
OxyContin binds to opioid receptors in the brain, altering how pain is perceived and triggering the release of dopamine, which reinforces drug-seeking behavior.
3. What does OxyContin look like?
Being able to identify OxyContin is important. The drug is available in tablet form, typically round or oval-shaped, and comes in different colors depending on the dosage. It often has an imprint indicating the strength and brand.
4. What are the early signs of oxycodone addiction?
Early oxy symptoms include increased tolerance, withdrawal symptoms, neglect of responsibilities, and persistent cravings.
Reclaim Your Life From OxyContin Addiction With Lumina Recovery
OxyContin addiction can disrupt lives, but recovery is possible with the right support and treatment. Recognizing the signs and risk factors for oxycodone addiction and taking proactive steps toward treatment can provide hope for those ready to recover.
Our medically supervised detox program ensures a safe and supportive withdrawal process, while our specialized treatment for prescription drug and opioid addiction addresses both the physical and psychological aspects of dependency. Through evidence-based therapies and personalized care, we help individuals break free from addiction and regain control of their lives.
Start your recovery journey today. Contact us to learn how we can support you or your loved one in overcoming OxyContin addiction and building a healthier future.
Sources:

Professions With the Highest Substance Abuse Rates
When it comes to substance abuse, some professions report higher rates than others. Various factors, including job-related stress, accessibility to substances, and the nature of the work itself can influence jobs with the highest substance abuse issues. Understanding which professions are more vulnerable can help in creating targeted support and intervention strategies.
The Substance Abuse and Mental Health Services Administration (SAMHSA) published results from the National Survey on Drug Use and Health (NSDUH) in 2015. It reported substance use disorder by industry, providing valuable insights on the general population of professions with the highest rate of substance abuse from 2008 to 2012.1
Impact of Substance Abuse in the Workplace
Substance use has a profound negative impact on industries across the United States, manifesting in several costly ways. The repercussions are far-reaching, affecting not only individual employees but also the overall productivity and financial health of companies.
Annually, U.S. businesses lose billions of dollars due to issues related to employees’ alcohol and drug use. The losses stem from various factors:
Lost productivity. Substance use can significantly diminish an employee’s ability to perform their duties efficiently, leading to reduced output and quality of work.
Workplace accidents and injuries. Impairment due to substance use increases the risk of accidents and injuries in the workplace, which not only endangers the affected employee but can also pose risks to their coworkers.
Employee absenteeism. Increased absenteeism is common among employees dealing with substance abuse as they may miss work due to the effects of their substance use or related health issues.
Low morale. Substance abuse can affect the morale of the entire team, not just the individual struggling with substance use. The behavior of one affected individual can impact the dynamics and overall mood of the workplace.
Increased illness. Health problems associated with drug and alcohol use can lead to increased medical claims and higher healthcare costs for employers.
Highest Rates of Heavy Alcohol Use by Industry
Substance abuse manifests distinctly across various industries, with heavy alcohol use being a significant concern. The data highlights industries that report the highest rates of heavy drinking within the past month among their workforce and underscores the need for industry-specific strategies to address and reduce alcohol consumption.
- Mining – 17.5%
- Construction – 16.5%
- Accommodations and food services – 11.8%
- Arts, entertainment, and recreation – 11.5%
- Utilities – 10.3%
Highest Rates of Illicit Drug Use by Industry
Illicit drug use within the workforce poses critical challenges for employers, impacting safety, productivity, and the overall workplace environment. Industries with the highest rates of past month illicit drug use point to sectors where targeted interventions and policies are crucial to combat this issue effectively.
- Accommodations and food services – 19.1%
- Arts, entertainment, and recreation – 13.7%
- Construction – 12.1%
- Management – 12.1%
- Information – 11.7%
Highest Rates of Substance Use Disorder by Industry
Substance use disorder (SUD) involves recurrent use of alcohol or drugs that causes clinically significant impairment. The high rates of substance use disorder by industry show a profound impact on both individual and organizational levels.
- Accommodations and food services – 16.9%
- Construction – 14.3%
- Arts, entertainment, and recreation – 12.9%
- Mining – 11.8%
- Utilities – 11.5%
- Management – 11.4%
Potential Factors for High Substance Abuse Rates

Stressful working conditions, often characterized by high-stress demands and low control, can lead to substance use as employees seek relief from constant pressure. Long hours and irregular shifts can disrupt normal sleep patterns and social lives, increasing reliance on substances as a coping mechanism for stress and fatigue.
Poor management and job dissatisfaction can further exacerbate these issues, as employees may feel undervalued or unsupported. In some sectors, such as hospitality or entertainment, alcohol and drugs are more readily available and may be integrated into the social fabric of the workplace, presenting frequent opportunities for misuse. Repetitive work and boredom can lead to substance use as a form of escapism.
Dual Diagnosis Care: Treating the Whole Person
Dual diagnosis care is a holistic and integrated treatment approach designed to address the complex needs of individuals who experience both substance use disorders and mental health issues, such as stress, anxiety or depression, simultaneously.
This well-rounded method is crucial because it acknowledges that both conditions can deeply influence each other and need to be treated concurrently to enhance the effectiveness of recovery and reduce the risk of relapse.
The Importance of Integrated Treatment
Traditional treatment methods that address only one issue at a time are less effective for individuals with dual diagnosis. Integrated treatment plans are tailored to treat both mental health and substance use disorders together.
Therapies like cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), or other psychotherapies help manage mental health symptoms and develop coping mechanisms for dealing with both disorders.
Medication management can help stabilize mood or treat mental health symptoms while managing withdrawal symptoms and cravings associated with substance use.
Support groups can help one engage with others who face similar challenges and provide social support and insights into successful strategies for managing dual diagnosis.
Incorporating holistic therapies and strategies such as mindfulness, meditation, and yoga can improve overall mental health and well-being.
Treating the Root Causes
To effectively treat dual diagnosis, it is essential to get to the root of the problem. This means understanding the underlying causes of both mental health issues and substance use disorder.
Treatment must go beyond mere symptom management and strive to resolve the core psychological and emotional issues contributing to the disorders. A thorough assessment by trained professionals helps in identifying these underlying factors, which might include trauma, stress, or genetic predispositions.
Find the Right Support With Lumina Recovery
Substance abuse affects those in lots of different professions, but we can see higher rates in certain industries which may in part be due to their specific work environments and job demands. By addressing the root causes of stress and providing supportive and healthy ways to cope, it is possible to reduce these rates.
Lumina Recovery provides treatment options for many groups of people dealing with substance abuse issues, including dual diagnosis care and specialized executive addiction treatment. Remember, asking for help is a sign of strength, not weakness.
If you need support in managing substance abuse, don’t hesitate to contact us today.
Source:

How Long Does OxyContin Stay in Your System?
OxyContin, a powerful prescription medication to manage pain, falls under the class of drugs known as opioids and contains the active ingredient oxycodone.
Understanding the effects of OxyContin on the body, its half-life, and the factors that influence its length of time in the system is essential for those fighting and their loved ones.
The Timing and Effects of OxyContin
Oxycodone is a potent opioid medication used to manage moderate to severe pain. Given its strength and potential for addiction, it’s important to know how quickly it acts, how long it stays in the system, and its half-life.
How long does it take for OxyContin to work?
The onset of oxycodone’s effects depends on several factors but largely on the formulation of the medication. For immediate-release oxycodone formulations, such as OxyContin, the active ingredient oxycodone begins to relieve pain within 10 to 30 minutes of oral ingestion.1
This rapid onset makes it a preferred option for acute pain management, post-operative pain, or breakthrough pain that occurs despite round-the-clock opioid therapy.
How long does OxyContin last?
The duration of pain relief provided by oxycodone varies based on its formulation.
Immediate-release formulations offer pain relief for about three to six hours. These are usually prescribed for pain that is expected to last for a short period or for pain that comes and goes.1
Extended-release formulations are designed to provide pain relief for up to 12 hours. This type of oxycodone is used for ongoing, chronic pain, providing a steady level of medication in the body over an extended period.1
Patients are advised to follow their prescription guidelines closely to avoid the risk of overdose or increased dependency due to the potent nature of oxycodone.
What is the half-life of OxyContin?
The half-life of oxycodone is approximately three to five hours in healthy adults, which means it takes about that time—three to five hours—for the concentration of the drug in the blood to reduce by half.
The drug’s half-life can vary based on several factors, including liver function, age, and overall health. The half-life of a drug is a critical factor in determining how frequently a dose should be taken and plays a key role in decisions regarding pain management protocols.1
Detection Timelines for OxyContin
Oxycodone’s detectability depends on the type of test being used:
- Urine Tests: Oxycodone can be detected in urine from about one to three days after the last dose. This window can vary depending on the individual’s metabolism and the frequency of use.3
- Blood Tests: Oxycodone appears in the blood shortly after ingestion and can generally be detected for up to 24 hours post-administration.2
- Saliva Tests: These tests can detect oxycodone within minutes of use and up to 36 hours after last use.3
- Hair Follicle Tests: Although not as commonly used for routine screening due to their higher cost and longer result times, oxycodone can be detected in hair for up to 90 days after the last dose, providing a much longer window of detectability.3

7 Factors Influencing the Duration of OxyContin in the System
Several physiological and lifestyle factors can affect how long oxycodone stays in an individual’s system:2
- Metabolic Rate: Individuals with a higher metabolic rate tend to process and eliminate substances like oxycodone faster than those with a slower metabolism.
- Age: Older adults generally have a slower metabolism, which means oxycodone may stay in their system longer compared to younger individuals.
- Body Mass and Composition: Body fat percentage and overall body mass can influence how drugs are metabolized and excreted. Oxycodone, being slightly lipophilic, might linger longer in individuals with higher body fat.
- Liver and Kidney Health: The liver metabolizes oxycodone, and the kidneys are responsible for excreting it. Any liver or kidney impairments can delay this process, thereby prolonging the presence of oxycodone in the body.
- Dosage and Frequency of Use: Higher doses and more frequent usage can increase the amount of time oxycodone is detectable in the system. Chronic use can lead to accumulation in the body, resulting in longer detection times.
- Hydration and Diet: Hydration levels can affect the concentration of oxycodone in urine, while certain foods and supplements might interact with drug metabolism.
- Concurrent Medications: Some medications can induce or inhibit the enzymes that metabolize oxycodone, thus affecting how quickly it is cleared from the body.
Seeking Help for OxyContin Abuse
If you or someone you care about is struggling with OxyContin use, it’s crucial to recognize when it’s time to seek help. Signs of abuse might include using more of the drug than prescribed, a preoccupation with obtaining and using the drug, or continuing use despite negative consequences in personal health, relationships, and responsibilities. Acknowledging these signs is the first step toward recovery.
Various resources are available for those facing challenges with OxyContin. Prescription drug treatment programs can range from medical detoxification and inpatient rehab programs to outpatient therapy and support groups. The right approach depends on the individual’s specific needs and circumstances. Consulting a healthcare provider can start the process of recovery. Remember, seeking help is a sign of strength and the first step towards reclaiming control of your life.
Take the Step Toward Healing From OxyContin With Lumina Recovery
Understanding how OxyContin affects the body and how long it stays in the system is fundamental for those prescribed this medication and for those who may be struggling with its use. While the medication is effective for pain management, its potential for dependence requires careful consideration and management.
Lumina Recovery’s opioid addiction treatment program provides every step of support from detoxification to residential inpatient programs to telehealth services.
If opioid addiction is impacting your life and feels overwhelming, don’t hesitate and reach out to Lumina Recovery today to start your journey back to health.
Sources:

A Legal Professional’s Guide to Addiction Recovery
Addiction impacts individuals from all walks of life in any profession, including those in high-pressure careers such as law. Legal professionals, from attorneys to judges, are particularly susceptible to the stress and demands of their jobs, which can sometimes lead to substance use disorders.
This guide is tailored to help individuals within the legal profession understand the nuances of addiction in their field, recognize the need for assistance, including executive addiction treatment, and take the initial steps toward recovery.
Addiction in Legal Professionals
A study by the Hazelden Betty Ford Foundation in collaboration with the American Bar Association sheds light on the sobering realities of addiction within the legal community. This research published in the Journal of Addiction Medicine involved a detailed survey of 12,825 lawyers across the United States. The findings revealed significant levels of substance abuse and mental health concerns among legal professionals:1
- Approximately 36.4% of the participants who responded to the initial set of questions on alcohol use demonstrated signs of alcohol abuse or dependency.
- When considering those who completed all alcohol-related questions, about 22.6% acknowledged problematic substance abuse.
- Some of the most common mental health issues reported by legal professionals in the survey were anxiety (61.1%), depression (45.7%), and bipolar disorder (2.4%).
Factors Contributing to High Rates of Addiction
High pressure and stress. Legal professionals often work in environments where high stress is the norm. Long hours, client demands, tight deadlines, and the high stakes of many legal outcomes can create a pressure cooker atmosphere. This intense stress can lead to substance use as a form of coping mechanism to ‘take the edge off’ or manage stress and anxiety.
Culture of alcohol consumption. The legal profession is also known for its robust drinking culture. Networking events, dinners with clients, and even casual meetings often occur in settings where alcohol is readily available. This normalization of alcohol can make it difficult for individuals to recognize the line between social drinking and problematic behavior.
Reluctance to seek help. There’s a significant stigma associated with admitting to substance abuse problems in a profession that prides itself on rationality and control. Many legal professionals fear that seeking help could jeopardize their careers, leading to a reluctance to address addiction issues until they become severe.
Impact of Addiction on Professional Life
The effects of substance abuse in the legal profession can be devastating, not only personally but professionally. Impaired judgment, decreased productivity, ethical breaches, and even legal ramifications like disbarment can result from unchecked addiction. The personal toll is equally harsh, with relationships, physical health, and mental well-being all suffering.
The Importance of Seeking Help
It is vital for anyone struggling with addiction, including legal professionals, to seek help. Addiction is a progressive illness that can lead to serious health complications, strained relationships, and a decline in job performance. The sooner one acknowledges the problem and seeks intervention, the better the chances of recovery and maintaining a successful career.
Addiction treatment for executives caters specifically to professionals, including legal practitioners, who are available and provide discreet, comprehensive support tailored to their unique needs. These programs address both the psychological and occupational challenges faced by legal professionals and offer strategies for managing stress in healthy ways.
4 Steps Toward Recovery for Legal Professionals
Recovering from addiction is a multifaceted process, especially within the legal profession where the stakes are high and the pressures are immense. Taking the right steps toward recovery can help you put yourself or your loved one on the road to specialized addiction treatment for a professional.
1. Acknowledging the Problem
The first and often hardest step is admitting there is a problem. For legal professionals, this means recognizing how their substance use has not only impacted their health but also their ability to perform their duties effectively.
Tip: Journaling can be a helpful tool. Writing down instances where substance use has affected your professional and personal life can make the issues clearer and strengthen your resolve to seek help.
2. Seeking Professional Help
Finding the right treatment program is crucial. For legal professionals, the ideal program is one that understands the specific challenges and triggers associated with the legal profession. Addiction treatment for professionals often offers a blend of medical detoxification, individual counseling, group therapy, and legal-specific support groups.
Resources to consider:
- Specialized Treatment Facilities: Some facilities offer specialized programs for executives and professionals, including lawyers, where confidentiality and discretion are a top priority.
- Therapists and Psychiatrists: Professionals who specialize in addiction and understand the unique pressures of the legal field.
- Lawyer Assistance Programs: Most state bar associations have a lawyer assistance program that provides confidential support to legal professionals dealing with addiction.

3. Support Networks
Building a robust support network is essential. This network should include peers who understand the pressures of the legal profession, as well as family and friends who can offer emotional support.
Networks Include:
- Professional Groups: Organizations like Lawyers Concerned for Lawyers (LCL) provide a community of peers who share similar experiences and challenges.
- Support Groups: Joining groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) can provide ongoing support and accountability.
- Family and Friends: Educating your closest circle about your challenges and recovery process can ensure they provide the right kind of support.
4. Ongoing Management
Recovery does not end with treatment—it is a lifelong process of managing one’s well-being. For legal professionals, ongoing management often includes stress reduction techniques, regular check-ins with mental health professionals, and sometimes, career adjustments to reduce stress.
Consider these strategies:
- Mindfulness and Meditation: Practices like meditation and mindfulness can help manage stress and reduce the likelihood of relapse.
- Regular Exercise: Physical activity is a proven stress reliever and mood booster.
- Time Management: Implementing effective time management strategies can help prevent work overload, a common trigger for substance use.
- Professional Boundaries: Setting clear professional boundaries can help manage work-related stress and prevent burnout.
Take the First Step Towards Sobriety With Lumina Recovery
Addiction within the legal profession is a significant issue that demands attention and action. By understanding the unique challenges faced by legal professionals and emphasizing the importance of seeking help, we can mitigate the impacts of addiction in the legal field.
Lumina Recovery’s specialized program for executives is ready to provide support and confidentiality at any point of the recovery journey from initial detox and dual diagnosis to sober living. Seeking help is a sign of strength, not weakness, and it is the first step toward a healthier, more sustainable career in law.
Take the first step towards a healthier future today. Reach out for support and begin your journey to recovery.
Sources:

Understanding Drug Abuse Among Older Adults
As the population ages, the complexities of managing health conditions increase, often leading to the use of multiple medications. While prescription medications are necessary for treating various ailments, there’s a growing concern about the abuse of these drugs among older adults.
However, it’s not just prescription medications that pose a risk; alcohol and even some over-the-counter medications also frequently contribute to substance abuse issues in this demographic.
Understanding the scope and impact of these commonly abused substances is crucial for developing effective prevention and management strategies. This understanding helps ensure that older people can enjoy a higher quality of life, free from the constraints of substance abuse.
Commonly Abused Drugs
As older adults age, they often experience a range of health issues that necessitate the use of multiple medications and can lead to substance use disorders. Understanding the most commonly abused drugs in this demographic from the National Institute on Drug Abuse is essential for prevention and management.1
Alcohol
What drug is most commonly abused by older adults? Alcohol. The National Institute on Alcohol Abuse and Alcoholism shows that 20% of the age group 60-64 years and 10% of 65 years and older report binge drinking.2
Alcohol and prescription drugs are commonly used together, which can significantly increase the risk of adverse interactions. Alcohol can exacerbate the effects of medications, increasing sedation and confusion, and complicate the management of chronic conditions.
Prescription Opioids
Opioids are one of the most commonly prescribed medications by healthcare providers for pain management in millions of adults aged 65 years and older, particularly for chronic conditions such as arthritis, cancer pain, and neuropathic pain.1
Drugs like oxycodone, hydrocodone, and fentanyl offer effective pain relief but also pose a high risk of misuse of prescription drugs and overdose. Due to their age-related slower metabolism and organ function, older patients may experience prolonged drug effects and side effects, increasing the risk of dependency.
Marijuana
The legalization and increasing social acceptance of marijuana have led to its rising use among older adults for both medicinal and recreational purposes. While marijuana can provide benefits such as pain relief and reduction in anxiety, it also carries risks, particularly when used in conjunction with other medications.1
For older individuals, the psychoactive effects of THC, the primary active compound in marijuana, can exacerbate cognitive impairments and lead to confusion, disorientation, and memory lapses. Additionally, marijuana in any form from dabs to edibles can interact with prescription medications like blood thinners, antidepressants, and anxiety medications.
Benzodiazepines
Benzodiazepines are frequently prescribed to treat anxiety, insomnia, and even muscle spasms in older patients. Medications like lorazepam (Ativan), diazepam (Valium), and alprazolam (Xanax) are effective for short-term relief but are associated with a high risk of substance use disorders.1
Prolonged use can lead to tolerance, requiring higher doses to achieve the same effects, and can severely impact cognitive function, increasing the risk of falls and accidents.
Antidepressants
While generally less addictive, antidepressants for mental health can still be misused by older adults, particularly when they are taken without proper medical supervision or in conjunction with other medications.
SSRIs (selective serotonin reuptake inhibitors) and SNRIs (serotonin and norepinephrine reuptake inhibitors) can interact with other drugs, leading to increased side effects or diminished effectiveness of treatment programs.
Over-the-Counter (OTC) Medications
Older adults might also misuse over-the-counter medications, including sleep aids and cold medicines. Products containing antihistamines or cough suppressants can be problematic due to their sedative properties, which can be intensified in older bodies.2
The Risk of Polypharmacy
Polypharmacy refers to the concurrent use of multiple medications by a patient, typically to manage several health conditions simultaneously. This practice is particularly prevalent among aging baby boomers, who often have multiple chronic diseases requiring various treatments. While necessary for managing these conditions, polypharmacy significantly increases the complexity of care, heightening the risk of drug interactions and adverse effects.
The use of numerous medications can lead to a higher likelihood of adverse drug reactions. Each additional medication not only adds a potential for interactions that can diminish the effectiveness of treatments but also increases the risk of severe side effects. These interactions can cause unexpected health issues such as increased blood pressure, kidney damage, or gastrointestinal distress.
The integration of recreational drugs like alcohol and marijuana into an older adult’s regimen compounds the risks associated with polypharmacy. These substances can interact with prescription medications, potentially leading to enhanced sedative effects, altered drug metabolism, and increased cognitive impairment. Such interactions are particularly dangerous for the elderly, whose organ function may already be compromised.

Population-Specific Effects
The effects of drug abuse can be more pronounced in older adults due to several age-related physiological changes:
- Metabolism and Excretion
As the body ages, liver and kidney functions slow down, affecting how medications are metabolized and excreted. This can lead to drugs staying in the body longer, increasing the risk of side effects and complications.1
- Increased Sensitivity
Older adults often exhibit increased sensitivity to medications due to decreased body water, increased fat storage, and changes in the central nervous system. These changes can amplify the effects of drugs, making therapeutic doses potentially harmful.
- Cognitive and Physical Health
The impact of drug abuse can exacerbate existing health problems. Cognitive impairments can worsen, leading to poor decision-making and difficulties with daily living activities. Physically, the risk of falls and other injuries increases, potentially leading to a cycle of increased medication use to manage pain from such injuries.
Supporting Older Individuals Abusing Drugs
Supporting elderly individuals struggling with drug abuse requires a comprehensive and compassionate approach tailored to their unique needs. Recognizing signs of substance abuse in older adults, such as changes in behavior, isolation, or neglect of personal hygiene, is critical for early intervention.
Medical evaluation and health care are essential to determine the extent of the abuse and any underlying health issues. Treatment options include medically supervised detoxification, inpatient or outpatient rehabilitation, and therapy such as cognitive behavioral therapy (CBT).
Regular medical reviews, patient and caregiver education, and the use of support groups and community resources are also crucial to effectively support recovery and improve the quality of life for elderly individuals facing substance abuse issues.
Explore Options for Elderly Drug Abuse With Lumina Recovery
Addressing drug abuse among older adults demands a nuanced understanding of the unique challenges and risks they face. By fostering a compassionate and informed approach, we can significantly mitigate the impacts of drug abuse in older adults and promote healthier, safer aging for all.
Lumina Recovery’s specialized program for seniors and older adults provides optimal support for the older population dealing with an addiction to prescription drugs or alcohol.
Learn more about your options with specialized programs that effectively address prescription drug abuse in older adults. Ensure a healthier, safer aging process with informed, compassionate care.
Sources:
Additional Resources
Once you have completed your rehabilitation program at one of our drug and alcohol treatment centers, you should try to surround yourself with people who can encourage you to stay sober. Many people find that support groups are the best source of encouragement. You can find hundreds of support groups and meetings in your community. Our drug addiction treatment centers stress the importance of personal chemical dependency resources, especially when you are new to sobriety. Below are various addiction and mental health resources for people in recovery who want additional support.
Christian Addiction Recovery Resources
Our substance abuse services aren’t limited to specific programs, but rather we believe in the importance of incorporating faith-based programs to promote spiritual healing, like our Faith in Recovery program.
With that said, below are some faith-based addiction recovery resources that could help you in your spiritual healing from addiction:
- Battlefield of the Mind by Joyce Meyer
- Boundaries by Dr. Henry Cloud & Dr. John Townsend
- Christian Families in Recovery: A Guide for Addiction, Recovery, and Intervention Using God’s Tools of Redemption by Robert and Stephanie Tucker
- Club New Life Christian Ministry for Addiction and Recovery
- Lost & Found: Recovery in Christ by Bruce Stanley
- Overcoming Emotional Obstacles through Faith: Navigating the Mind Field by Anthony Acampora, Director of Banyan’s Faith in Recovery Program
- The Case for Christ by Lee Strobel
Mental Health Resources for Recovery
Lumina Recovery consist of both mental health and substance abuse treatment facilities, meaning we offer mental health resources as well as chemical dependency resources. What’s more, addiction often co-occurs with mental illness, making these resources ever more important.
Below are some resources for mental health recovery that can help you or your loved one:
- This Emotional Life video series
- No Kidding, Me 2!! with Joe Pantoliano
- Dare: The New Way to End Anxiety and Stop Panic Attacks by Barry McDonagh
- Pleasure Unwoven: An Explanation of the Brain Disease of Addiction by Kevin McCauley
- Declutter Your Mind: How to Stop Worrying, Relieve Anxiety, and Eliminate Negative Thinking by S.J. Scott and Barrie Davenport
Call Us Today – (877) 716-7515

